SINDROMI MIELODISPLASTICHE · • Le mielodisplasie sono patologie clonali caratterizzate dalla...
Transcript of SINDROMI MIELODISPLASTICHE · • Le mielodisplasie sono patologie clonali caratterizzate dalla...
• Uomo di 70 aa
• APR: gastrite cronica, ipertensione arteriosa
• Sintomi: astenia
• Hb 9g/dL; MCV 108; GB 2.100 mm3; PLT 83.000; LDH 400; bilirubina ind. 2
• Reticolociti bassi
• Vit B12, folati, bilancio marziale nella norma
• A. midollare: mielodisplasia
• Le mielodisplasie sono patologie clonali caratterizzate dalla displasia midollare che determina emopoiesi inefficace
• Midollo ricco displastico
• Pancitopenia periferica
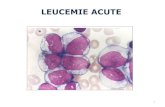
• Evoluzione clonale in leucemia acuta
Epidemiology of MDS
• Incidence:
– overall: 5/100.000/year
– ≥65yrs: 20-50/100.000/year
• Proportion of people aged >65yrs in Europe: 14%
• Expected new cases of MDS each year in Europe: ~15.000
• Standardized Mortality Ratio (SMR) in MDS is 7.30 with respect to the general
population
J Clin Oncol 2005;23:7594-7603
CELLULA STAMINALE TOTIPOTENTE
LINFOPOIESI
CELLULA STAMINALE MIELOIDE CFU-GEMM
LINEA ERITROIDE MEGACARIOCITI
GLOBULI ROSSI PIASTRINE
BFU-E CFU-Me
COLONIE
GRANULOCITO-
MACROFAGICHE
CFU-GM
CFU-M
MACROFAGI
CFU-G
GRANULOCITI
Morphological score Dyserythropoiesis
Multinuclearity Nuclear lobulation
Megaloblastosis
Pyknosis Defective
hemoglobinisation and
cytoplasmic fraying
Ring sideroblasts
Leukemia, 2015
Morphological score Dysgranulopoiesis
Myeloblast Auer rod Hypolobulation
Abnormal nuclear shape Hypogranulation
Leukemia, 2015
Morphological manifestations of dysplasia Dysmegakaryocytopoiesis
Micromegakaryocytes
Nuclear hypolobation
Multinucleation
Cause di mielodisplasia
• Virus
• Meccanismi immunologici
• Fattori tossici ambientali
• Benzene, sostanze chimiche
• Radiazioni
• Chemioterapici ( alchilanti, epipodofilotossine)
CRITERI CLASSIFICATIVI PER LE MIELODISPLASIE
MORFOLOGICI
displasia
blasti
sideroblasti ad anello
ANOMALIE CITOGENETICHE
ANOMALIE MOLECOLARI
MDS WHO 2016
• MDS with single lineage dysplasia (MDS-SLD)
• MDS-SLD with ring sideroblasts
• MDS with multilineage dysplasia –MDS-MLD with ring sideroblasts
• MDS with isolated del(5q)
• MDS with excess blasts –MDS-EB1
–MDS-EB2
• MDS, unclassifiable (MDS-U)
Either ≥15% RS or 5% RS
and SF3B1 mutation
The lineages manifesting significant morphplogic
dysplasia
frequently do not correlate
with the specific cytopenias
in individual MDS cases
BLOOD, 19 MAY 2016 x VOLUME 127, NUMBER 20
• Female preponderance
• 5q- sole karyotypic abnormality
• macrocytic anemia (MCV > 100 fL)
• high platelet count
• megakaryocytes with monolobulated nuclei
• prolonged survival
Distinct haematological disorder with
deletion of long arm of No. 5 chromosome
(Van den Berghe H. et al., Nature 1974)
miRNA-145
miRNA-146a RPS14
Nature 2008;451:335; Nat Med 2010;16:49; Nat Med 2010;16:59; Cancer Cell. 2014;26:509-20.
P53/Glycophorin
CSNK1A1
Insights into the molecular basis of
MDS with isolated del(5q)
Vulnerability of 5q- clone to lenalidomide
consequent to gene haploinsufficiency
http://www.cell.com/cancer-cell/abstract/S1535-6108(14)00335-3
WHO 2016
• MDS with single lineage dysplasia (MDS-SLD)
• MDS-SLD with ring sideroblasts
• MDS with multilineage dysplasia –MDS-MLD with ring sideroblasts
• MDS with isolated del(5q)
• MDS with excess blasts –MDS-EB1
–MDS-EB2
• MDS, unclassifiable (MDS-U)
WHO 2008 translation
= RCUD
= RARS
= RCMD
= RCMD-RS
= RAEB-1
= RAEB-2
QUADRO CLINICO e DI LABORATORIO
• ANEMIA MACROCITICA (MCV 105), reticolociti bassi
• PIASTRINOPENIA
• NEUTROPENIA
• IPER FERRITINEMIA
• SPLENOMEGALIA
• LDH alte, aumento bilirubina indiretta
LA CITOPENIA E’ DI SEVERITA’ MOLTO VARIABILE E PUO’ COINVOLGERE UNA O PIU’ LINEE
CITOPENIA
SOSPETTO DIAGNOSTICO MA… MANDATORIO ESCLUDERE ALTRE CAUSE
Blood tests
• WBC, Hb, PLT count, MCV, reticulocyte, PB smear;
• S-folic acid, cobalamin;
• Iron, TIBC, ferritin;
• LDH, bilirubin, haptoglobin, Coombs test;
• ALT, AST, Albumin, S-protein electrophoresis;
• Uric acid, Creatinine, S-erythropoietin;
• Thyroid function tests;
• Anti-HIV, anti-Parvovirus B19, CMV-test; PNH clone
• Exclude thalassemia / hemoglobinopathy.
Proposal for standardized diagnostic procedures in MDS
Diagnosis of Myelodysplastic Syndrome
Bone Marrow Peripheral Blood
Morphology
Cytogenetic Analysis
• Bone marrow dysplasia is not specific for MDS
• Morphological BM evaluation is dependent form sample quality
• Evaluation of dysplasia may be hampered by the presence of hypocellularity or fibrosis (15-20% of MDS cases)
• Three months observation
TERAPIA CURATIVA:TMO ALLOGENICO
Uomo 30 aa
• MDS-EB2 (blasti 18%)
• Hb 6; PLT 30.000; GB 1000
• MDS-MLD
• Hb9.5; PLT 120.000; GB 900
Uomo 85 aa
• MDS-SLD
• Hb 7; PLT 200.000; GB 5000
Survival of MDS patients classified according to WHO subgroups
J Clin Oncol 2005;23:7594-603
Overall survival (P<.001)
Leukemia-free survival (P <.001)
International Prognostic Scoring System (IPSS)
Score
0 0.5 1.0 1.5 2.0
Medullary blasts (%) < 5 5–10 – 11–20 21–30
Karyotype Good* Intermediate† Poor‡ – –
Cytopenia 0/1 2/3 – – –
Low risk 0 points
Intermediate-1 0.5–1.0 points
Intermediate-2 1.5–2.0 points
High risk ≥ 2.5 points
Greenberg P, et al. Blood. 1997;89:2079-88.
*Good: normal, -Y, del(5q), del(20q). †Intermediate: other abnormalities not seen in “good” or “poor”. ‡Poor: complex (≥ 3 abnormalities) or chromosome 7 anomalies.
International Prognostic Scoring System (IPSS)
Punteggio Rischio Sopravvivenza
mediana
0 Basso 5.7 anni
0.5-1.0 Intermedio 1 3.5 anni
1.5-2.0 Intermedio 2 1.2 anni
≥2.5 alto 0.4 anni
Blood 1997;89:2079-2088
International Prognostic Scoring System for MDS
Variable 0 0.5 1 1.5 2
BM blasts % <5 5-10 - 11-20 21-30
Karyotype* Good Intermediate Poor
Cytopenias° 0/1 2/3
*Good: normal, -Y, del(5q), del(20q); Poor: complex,
chromosome 7 anomalies; Intermediate: other
abnormalities.
°Hemoglobin < 10 g/dL, absolute neutrophil count <
1,500/µL, platelet count < 100,000/µL.
Scores for risk groups are as follows: Low, 0; INT-1,
0.5-1.0; INT-2, 1.5-2.0; and High, 2.
citogenetica
Very good good intermediate poor very poor del (11q) normal -7/7q del(q21) >3 anomalie
-Y del(1;7) +8 del(q26)
del (5q) i(17q) -7/7q et al
del (12p) +19 3 anomalie
del (20q) +21
del (5q) et al ogni doppia
Prognosi Very good 60.8 mesi OS
Good 48.5 mesi
Intermediate 24 mesi
Poor 14 mesi
Very poor 5.7 mesi
Shanz EHA 2010
TERAPIA CURATIVA:TMO ALLOGENICO
Uomo 30 aa
• MDS-EB2 (blasti 18%)
• Hb 6; PLT 30.000; GB 1000
• MDS-MLD
• Hb9.5; PLT 120.000; GB 900
• Cariotipo complesso
Int-2; survival 1.2aa
Uomo 85 aa
• MDS-SLD
• Hb 7; PLT 200.000; GB 5000
• 46 XY
Low risk; survival 5.7 aa
Frequency of somatic mutations in MDS
Papaemmanuil et al. Blood. 2013;122:3616-27
SF3B1-SRSF2 splicing
TET2 DNMT3A metilation
Relationship between SF3B1 mutation and ring sideroblasts
Quantitative enumeration
of ring sideroblasts
(325 MDS patients)
31% patients
with mutation in SF3B1
97% patients with RS,
3% patients no RS
SF3B1 mutation: positive predictive value for ring sideroblasts 97.7%
Absence of ring sideroblasts: negative predictive value
for SF3B1 mutation 97.8%
P=0.002
RARS, RCMD-RS
35% RA/RCMD/MDSdel(5q)/RAEB
Malcovati et al. Blood 2011;118:6239-46
Prognostic value of SF3B1 mutations
in patients with MDS and RS
Overall Survival
HR .37, P=.003
CI of Disease Progression
HR .31, P=.018
HR .27, P=.007 HR .22, P=.026
RA
RS
/RC
MD
-RS
A
ll W
HO
cate
go
ries
Malcovati et al. Blood. 2015 May 8
Relationship between SF3B1 mutation and ring sideroblasts
Quantitative enumeration
of ring sideroblasts
(325 MDS patients)
31% patients
with mutation in SF3B1
97% patients with RS,
3% patients no RS
SF3B1 mutation: positive predictive value for ring sideroblasts 97.7%
Absence of ring sideroblasts: negative predictive value
for SF3B1 mutation 97.8%
P=0.002
RARS, RCMD-RS
35% RA/RCMD/MDSdel(5q)/RAEB
Malcovati et al. Blood 2011;118:6239-46
MDS WHO 2016
• MDS with single lineage dysplasia (MDS-SLD)
• MDS-SLD with ring sideroblasts
• MDS with multilineage dysplasia –MDS-MLD with ring sideroblasts
• MDS with isolated del(5q)
• MDS with excess blasts –MDS-EB1
–MDS-EB2
• MDS, unclassifiable (MDS-U)
Either ≥15% RS or 5% RS
and SF3B1 mutation
Expected advantages of a molecular
classification
• High accuracy of class prediction (robust biomarkers regardless of morphological criteria).
• Identification of biologically homogeneous entities (more homogeneous prognosis, restricted patterns of clonal evolution).
• Ideal frame for development of targeted therapies and identification of specific mechanisms of resistance to treatment.
OS secondo rischio MDS-CI nei rischi WPSS basso (A), intermedio (B), alto e molto alto (C-D)
MDS a basso rischio
MDS ad alto rischio
TERAPIA
• Eritropoietina 30-40.000 U/sett (epo<500) (IPSS low int-1)
• Supporto trasfusionale
• Ferrochelazione
• 5azacitidina (IPSS-int2 high)
• Lenalidomide (5q-)
• Trapianto allogenico di midollo osseo
• 80 aa
• Cardiopatia ischemica
• Hb 7 g/dl; GB 4700 ANC 2700; PLT 270.00
• MDS-SLD con sideroblasti ad anello
• 46 XY
• IPSS low
TERAPIA
• Eritropoietina 30-40.000 U/sett (epo<500) (IPSS low int-1)
• Supporto trasfusionale
• Ferrochelazione
• 5azacitidina (IPSS-int2 high)
• Lenalidomide (5q-)
• Trapianto allogenico di midollo osseo
TERAPIA
• Eritropoietina 30-40.000 U/sett (epo<500) (IPSS low int-1)
• Supporto trasfusionale
• Ferrochelazione (deferoxamina, deferasirox)
• 5azacitidina (IPSS-int2 high)
• Lenalidomide (5q-)
• Trapianto allogenico di midollo osseo
TERAPIA
• Eritropoietina 30-40.000 U/sett (epo<500) (IPSS low int-1)
• Supporto trasfusionale
• Ferrochelazione
• 5azacitidina (ipometilante) (IPSS-int2 high)
• Lenalidomide (5q-)
• Trapianto allogenico di midollo osseo
OBIETTIVI DEL TRATTAMENTO IPOMETILANTE MIGLIORARE L’EMATOPOIESI RIDURRE O ANNULLARE IL FABBISOGNO TRASFUSIONALE ALLUNGARE LA SOPRAVVIVENZA GLOBALE
• 50aa
• APR CHT/RT neoplasia mammaria
• Hb 11g/dl; GB 2500 ANC 1100; PLT 110.000
• Cariotipo complesso
• MDS therapy related