Lez FA da T3tossicosi - TIM. Damiani 3/FA da T3 tossicosi.pdf · –comparsa improvvisa di...
Transcript of Lez FA da T3tossicosi - TIM. Damiani 3/FA da T3 tossicosi.pdf · –comparsa improvvisa di...
Caso Clinico
• Il paziente giunge in reparto per
– Cardiopalmo e dispnea da sforzo
– Astenia marcata, che aumenta nella giornata
– Dolori ai gruppi muscolari maggiori
• Non reperti di rilievo alla AF
– Modico fumatore (5-6 sigarette) dai 20 ai 35 anni
– Normale assunzione di vino ai pasti
Anamnesi patologica
• Diagnosi endoscopica di ulcera peptica circa 15 anni or sono risolta dopo un trattamento con anti-H2
• Sporadica assunzione di FANS (classici e Coxib) per dolori artrosici a carico del ginocchio destro
• Incidente stradale con frattura di clavicola e di tre coste l’anno scorso
Anamnesi patologica
• Sei mesi fa:– comparsa improvvisa di cardiopalmo, associato a
sensazione di vertigine ed a scotomi scintillanti dopo la colazione
– la moglie, infermiera, ha notato un polso celere ed irregolare e lo ha portato al pronto soccorso
Al Pronto Soccorso
• Conferma di polso aritmico con FC di ca 130 b/min (115 al polso periferico)
• Anisosfigmia del polso
• Non segni di scompenso cardiaco
• Normale l’esame obiettivo degli altri apparati
• Gli esami di laboratorio ed un ecocardiogramma eseguiti in urgenza escludono anemizzazione, disionie, danno miocardico acuto o patologia valvolare
Atrial Fibrillation
• AF is a common arrhythmia that may occur in paroxysmal and persistent forms.
• Paroxysmal AF may be seen in normal individuals, particularly during emotional stress or following surgery, exercise, acute alcoholic intoxication, or a prominent surge of vagal tone (i.e., vasovagal response).
• Persistent AF usually occurs in patients with cardiovascular disease, most commonly rheumatic heart disease, nonrheumatic mitral valve disease, hypertensive cardiovascular disease, chronic lung disease, atrial septal defect, and a variety of miscellaneous cardiac abnormalities.
• So-called lone AF, which occurs in patients without underlying heart disease, often represents the tachycardia phase of the tachycardia-bradycardia syndrome.
Morbidity associated with AF
1. Anxiety secondary to palpitations;
2. Excessive ventricular rate;this in turn may lead to hypotension, pulmonary congestion, angina pectoris, and in some patients can produce a tachycardia-mediated cardiomyopathy;
3. The pause following cessation of AF, which can cause syncope;
4. Loss of the contribution of atrial contraction to cardiac output, which may cause fatigue;
in patients with noncompliant ventricles and in mitral stenosis, the combination of the loss of the atrial contribution to ventricular filling and the abbreviated filling period due to the rapid ventricular rate in AF can produce marked hemodynamic instability, resulting in hypotension, syncope, or heart failure.
5. Systemic embolization, which occurs most commonly in patients with rheumatic heart disease;
Peters Ns et al. Lancet, 359:593, 2002
Principles of AF management
• Restoration of sinus rhythm– Electrical cardioversion
– Pharmacological cardioversion
• Maintenance of sinus rhythm– None or Drug treatment
– Permanent pacing, Radiofrequency ablation, Surgery
• Ventricular rate control– Calcium-channel blockers, Beta-adrenoceptor
antagonists, Digoxin, Antiarrhytmic drugs
• Reduction of thromboembolic risk– Warfarin or aspirin
Peters Ns et al. Lancet, 359:593, 2002
Trattamento del paziente
• Un ecocardiogramma trans-esofageo ha documentato l’assenza di trombi in atrio
• Alla luce di tale dato e della breve durata della AF il paziente e’ stato trattato con cardioversione elettrica con ripristino di un normale ritmo sinusale
• Il paziente e’ stato dimesso senza nessun trattamento farmacologico aggiuntivo
Decorso
• Dopo 3-4 settimane il paziente lamenta di nuovo la comparsa di episodi di cardiopalmo della durata di qualche ora
• Una registrazione ECG dinamica secondo Holter documenta la presenza di episodi parossistici di AF di durata variabile da pochi minuti a 4 ore
Nomenclature for Atrial Fibrillation
• Acute:– an episode of atrial fibrillation, usually within 48 h of its onset
• Paroxysmal:– intermittent, recurrent, and self-terminating
• Persistent:– will not self-terminate, but can be effectively cardioverted to sinus
rhythm
• Permanent:– atrial fibrillation that cannot be terminated by cardioversion, that
can be terminated only for brief intervals, or that lasts longer than 1 year without cardioversion having been attempted
• Chronic:– implies continuing atrial fibrillation and does not address the
important clinical distinctionbetween persistent and permanent atrial fibrillation
Peters Ns et al. Lancet, 359:593, 2002
Decorso
• Dopo 3-4 settimane il paziente lamenta di nuovo la comparsa di episodi di cardiopalmo della durata di qualche ora
• Una registrazione ECG dinamica secondo Holter documenta la presenza di episodi parossistici di AF di durata variabile da pochi minuti a 4 ore
• Per tale ragione il cardiologo che segue il paziente ha consigliato l’inizio di un trattamento con anticoagulanti orali in previsione di una seconda cardioversione. Un secondo cardiologo ha invece consigliato un trattamento con farmaci capaci di ridurre la frequenza.
Il paziente vi chiede.....
• E’ giusto fare una seconda cardioversione o e’ meglio usare farmaci?
• Ma la terapia anticoagulante e’necessaria e per quanto?
• Un mio amico usa l’aspirina. Perche’non posso farlo anch’io?
Risk factors for VTE in patients with AF
• Data from the Framingham study have shown that rheumatic heart disease that is complicated by AF is associated with a 18-fold increase in risk of TE.
• In patients without rheumatic heart disease, atrial fibrillation raises TE risk by a factor of about six. In these patients, incidence of ischaemic stroke without antithrombotic treatment is about 5% per year, but with large variation. Both TE risk and the contribution of AF to the causes of ischaemic stroke increase with age and comorbidity
Peters Ns et al. Lancet, 359:593, 2002
Risk factors for stroke, and indications for anticoagulation in patients with AF
• Age > 65 years
• Previous history of transient ischaemic attact or stroke
• History of hypertension
• Diabetes
• Heart failure
• Structural heart disease
• Rheumatic or other significant valvular heart disease
• Significant left ventricular systolic dysfunction
Peters Ns et al. Lancet, 359:593, 2002
Recommendations for AC for cardioversion of AF
• For elective cardioversion of AF of > 48 h duration start warfarin treatment (INR 2-3) three weeks before and continue for four weeks after cardioversion
• In urgent and emergency cardioversion administer iv Heparin followed by warfarin
• Treat atrial flutter similarly
• No AC treatment is required for SV tachycardia of AF of < 48 h duration
• Continue AC in patients with multiple risk factors or those at high risk of recurrent TE
ACCP Consensus Conference on AT Therapy, 2001
Practical guidelines for anti-thrombotic therapy in non-valvar AF
Lip GYH et al. BMJ, 325:1022, 2002
Practical guidelines for anti-thrombotic therapy in non-valvar AF
Lip GYH et al. BMJ, 325:1022, 2002
Nell’ ultimo mese....
• Il paziente e’ in trattamento con verapamil ed aspirina
• Continua a lamentare Cardiopalmo ed e’comparsa dispnea da sforzo
• Lamenta anche:
– Astenia marcata, che aumenta nella giornata
– Dolori ai gruppi muscolari maggiori
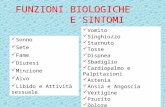
Principali manifestazioni cliniche dell’Ipertiroidismo
• Sintomi
– Astenia e debolezza muscolare– Mialgie– Irritabilita’– Intolleranza al caldo e diaforesi– Iperattivita’– Cardiopalmo– Aumento appetito– Riduzione del peso corporeo– Alterazioni mestruali e/o della
libido– In casi particolari disturbi cutanei
ed oculari
• Segni
– Tachicardia sinusale– Aritmie– Cute calda e sudata– Aumento della pressione
differenziale– Retrazione della palpebra e “lag lid”– Iperreflessia– Dolorabilita’ muscolare– Tremori– Onicolisi– In casi particolari variazioni di
volume della tiroide, oftalmopatia, dermopatia
Tests for thyroid dysfunctions
Thyroid Physiology
IODINEUPTAKE
TESTS RELATED TO CONCENTRATION OF THYROID HORMONES IN THE BLOOD
• Serum T3 and T4• Serum fT3 and fT4• Serum rT3• Serum TbG
TESTS THAT ASSESS METABOLIC IMPACT OF THYROID HORMONES
• Serum cholesterol• BMR
TESTS THAT ASSESS PITUITARY IMPACT OF THYROID HORMONES
• Serum TSH• TRH test
OTHER TESTS• TS Immunoglobulins• Anti TPO and TG antibodies
Valutazione dei vari tests di laboratorio nella diagnostica delle disfunzioni tiroidee
• T4 e/o T3 totali: da non utilizzare. Specificità e valore predittivo positivo troppo bassi
• Tiroxina libera (free-T4): specificità discreta. Rimangono alcuni problemi metodologici (gold standard “equilibrium dialysis”) che portano ad ampie variazioni inter-laboratorio. Non identifica la “T3-toxicosis” e puo’ dare falsi positivi nella “sick euthyroid syndrome”
• Tri-iodotironina libera (free-T3): non utilizzabile come test unico per sensibilità troppo bassa.
• TSH sensitive o supersensitive: buone sensibilità (89-95%) e specificità (90-96%). I falsi positivi sono spesso legati a farmaci (corticosteroidi)
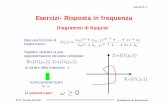
Relationships between fT4 and s-TSH levels in Thyroidal Disorders
Scientific American Medicine , 2003
s-TSH as Screening Test for Hyperthyroidism
“... sensitive TSH measurements are the single best screening test for hyperthyroidism.”
AACE Clinical Practice Guidelines for the Evaluation and Treatment of Hypertiroidism and Hypothyroidism, Washington, DC, 2002
Determinazione di fT4 e s-TSH nel paziente
• Free T4: 1.9 ng/dl V.N. 0.9-2.0
• s-TSH: <0.01 µg/dl V.N. 0.5-5.0
Come interpretare tale incongruenza?
s-TSH pittfalls
• TSH is not reliable in cases of suspected pituitary disease (FT4 is recommended).
• TSH may be an unreliable indicator of thyroid status in patients with acute severe nonthyroidal illness(e.g., CCU, ICU, acute severe psychiatric illness). In these cases FT4 is recommended.
• Within 3 months of a change in therapy for hyperthyroidism TSH may not reflect the clinical status. In these cases a FT4 test (or equivalent) or FT3 test (or equivalent) is recommended.
Subclinical Hyperthyroidism
• The combination of an undetectable serum thyrotropin concentration, as measured by an assay with a threshold of detection that is 0.1 mU per liter or less, and normal serum triiodothyronine and thyroxine concentrations (usually at the upper end of the normal range) is known as subclinical hyperthyroidism.
• When the lower limit of TSH is less than 0.4 mIU/L, 3.2% of the population is defined as having subclinical HT. If the diagnosis is limited to only those with TSH lower than 0.1 mIU/L the prevalence decreases to 0.7%.
• Subclinical HT is common in individuals treated with l-thyroxine being present in 14% to 21% of such patients.
Toft AD, N Engl J Med, 2001
Atrial fibrillation in subclinical hyperthyroidism
Perc
ent with A
trial Fibrillat ion
TSH <0.1 TSH 0.1-0.5 TSH >0.5
Serum TSH mU/L
Sawin et al, N Eng J Med, 331:1249, 1994
Subclinical hyperthyroidism and cardiovascular diseases
• 1191 old patients (>60 yrs) followed from 1988 to 1999 in Birmingham, UK
• Thyroid function tests (sTSH, fT4 e fT3) were measured in 1988
• Vital status was recorded on June 1 1999:
– phone call of survived patients
– ascertainment of date and cause of death for those who had died through the records of UK NHS Central Register
Parle et al, Lancet, 358:861, 2001
Subclinical hyperthyroidism and cardiovascular diseases
• During follow-up, 509 of 1191 people died, the expected number of deaths being 496 (standardised mortality ratio [SMR] 1.0, 95%CI 0.9–1.1).
• Mortality from all causes was significantly increased at 2 (SMR 2.1), 3 (2.1), 4 (1.7), and 5 (1.8) years after first measurement in those with low serum thyrotropin (n=71).
• Increases in mortality from all causes in years 2–5 were higher in patients with low serum thyrotropin than in the rest of the cohort (hazard ratios for years 2, 3, 4, and 5 were 2.1, 2.2, 1.8, and 1.8, respectively). This result reflects an increase in mortality from circulatory diseases (hazard ratios at years 2, 3, 4, and 5 were 2.3, 2.6, 2.3, 2.3), and specifically from cardiovascular diseases(hazard ratios at years 2, 3, 4, and 5 were 3.3, 3.0, 2.3, 2.2).
Parle et al, Lancet, 358:861, 2001
Kaplan-Meier survival curves according to serum TSH levels
Years of follow-up
Overa
ll surv
ival (%
)
Surv
ival fo
r CV d
iseases(%
)
Years of follow-up
Parle et al, Lancet, 358:861, 2001
Sensitive TSH Assay plus free-T4
Subnormal
Perform RAIU & SCAN(the majority of T3 toxicosis are due to iperactive thyroid nodules)
����/=Free T4
Borderline thyroid status
���� Free T3Suspect
T3 Toxicosis
���� Free T3 Pituitary Hypothyroidism
TSH afterTRH Test
Sick EuthyroidSyndrome
Diagnosis of Hyperthyroidism
Determinazione di fT4, fT3 e s-TSH nel paziente
• Free T4: 1.9 ng/dl V.N. 0.9-2.0
• s-TSH: <0.01 µg/dl V.N. 0.5-5.0
• Free T3: 2.5 ng/dl V.N. 0.2-0.6
La determinazione della free-T3 risolve la apparent e incongruenza: il paziente ha una “T3 tireotossicosi”
Caratteri distintivi della T3-tossicosi
• Prevale nei pazienti sopra i 60 anni ed e’ quasi sempre sostenuta da noduli autonomi
• Gli apparati maggiormente coinvolti sono:– Cardiovascolare:• Fibrillazione atriale e TPSV• Scompenso congestizio• Angina ed infarto
– Neuromuscolare:• Astenia e debolezza• Mialgie ed Atrofia muscolare (quadricipite)• Apatia, depressione, deterioramento cognitivo
– Gastroenterico:• Anoressia, stipsi e perdita ponderale
Diagnosi finale:
• Fibrillazione Atriale in paziente con Gozzo Nodulare (M. di Plummer) e T3-tireotossicosi
Letteratura di approfondimento:
• Editorial: Management of AF - Radical reform or modest modification? N Engl J Med 347:1883, 2002
• Peters NS et al. AF: strategies to control, combat and cure. Lancet 359:593, 2002
• Lip GYH et al. Antithrombotic therapy for AF. BMJ 325:1022, 2002
• Hegedus L: The thyroid nodule. N Engl J Med 351:1764, 2004
• Surks MI et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA 291:228, 2004






























































![SPETTOLI [modalit compatibilit ] ALLO... · cause accidentali o incidentali 2 causata da complicazioni ostetriche ... d’aborto 28 settimane: sincope, dolore retrosternale, cardiopalmo,](https://static.fdocumenti.com/doc/165x107/5c689a7e09d3f263648bbf56/spettoli-modalit-compatibilit-allo-cause-accidentali-o-incidentali-2-causata.jpg)