Leucemia Linfoblastica Acuta (adulto) - Siematologia · 2020. 7. 9. · Leucemia Linfoblastica...
Transcript of Leucemia Linfoblastica Acuta (adulto) - Siematologia · 2020. 7. 9. · Leucemia Linfoblastica...
-
Leucemia Linfoblastica Acuta
(adulto)
-
Classificazione delle leucemie linfoidi acute, WHO 2008
Leucemie linfoblastiche acute a cellule «precursor» B
• Leucemia/linfoma linfoblastica/o B, NAS
• Leucemia/linfoma linfoblastica/o B con anomalie genetiche ricorrenti
• Leucemia/linfoma linfoblastica/o B con t(9;22) (q34;q11.2);BCR-ABL1
• Leucemia/linfoma linfoblastica/o B con t(v;11q23); MLL riarrangiata
• Leucemia/linfoma linfoblastica/o B con t(12;21)(p13;q22); TEL-AML1(ETV6-RUNX1)
• Leucemia/linfoma linfoblastica/o B con iperdiploidia
• Leucemia/linfoma linfoblastica/o B con ipodiploidia
• Leucemia/linfoma linfoblastica/o B con t(5;14)(q31;q32);IL3-IGH
• Leucemia/linfoma linfoblastica/o B con t(1;19)(q23;p13.3); E2APBX1 (TCF3-PBX1)
Leucemie linfoblastiche acute a cellule «precursor» T
• Leucemia/linfoma linfoblastica/o T
Neoplasie a cellule B mature
• Linfoma di Burkitt (include anche la rara variante leucemica, L3 FAB)
NB Esistono poi forme miste, indifferenziate, bifenotipiche, bilineari…
-
LLA: Esami diagnostici
Sangue periferico:
Emocromo con formula leucocitaria ed esame morfologico (ematologo esperto) mediante striscio periferico
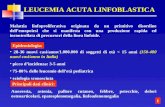
blasti > 2=% (leucocitosi non sempre presente, neutropenia, piastrinopenia, anemia)
Immunofenotipo (citometria a flusso): linea linfoide (CD13-; CD14-), linea B (CD10+, CD19+, CD20+, CD22+)
o T (CD1a+, CD3+, CD4+, CD7+, CD8+). Altri antigeni: CD34, HLA-Dr, TdT
Citogenetica/FISH e biologia molecolare: cromosoma Philadelphia / traslocazione BCR/ABL (30 % circa nel paziente
adulto;
va eseguita in tutti i pazienti indipendentemente dall’età, per la possibilità di terapia con TKI)
Aspirato midollare:
Striscio con mielogramma per valutazione (ematologo esperto)della percentuale di blasti midollari e della riserva
emopoietica
Citochimica: non più consigliata (puo’ essre utile la perossidai: negativa)
Immunofenotipo (citometria a flusso: linea linfoide (CD13-; CD14-), linea B (CD10+, CD19+, CD20+, CD22+)
o T ( CD1a+, CD3+, CD4+, CD7+, CD8+). Altri antigeni: CD34, HLA-Dr, TdT.
Citogenetica/FISH e biologia molecolare: cromosoma Philadelphia / traslocazione BCR/ABL
Biopsia osteomidollare:
Raramente necessaria (aspirato midollare povero di cellule) e nel caso immunoistochimica
NB. In tutti i pazienti es. del liquor (morfologico ed immuofenotipico)
-
LLA: Diagnostica avanzata
• Identificazione forme Ph-like (altri geni di fusione: potrebbero giovarsi di terapia con TKI come le LAL Ph+)
• Mutazione di IKZ (valore prognostico nelle forme sia Ph+che Ph-)
• TAC total body (nelle forme T massa mediastinica, nelle Burkitt-like o L3 masse toracoa-addominali)
• NGS (identificazione di sottogruppi di mutazioni sensibili a nuovi farmaci)
-
LLA: Follow-up
• Valutazione della minimal residual disease
(MRD), dopo consolidamento nelle forme Ph-, al
termine della prima fase di terapia con TKI, in
genere 80-90 giorni nelle Ph+.
• MRD: Ph+ molecolare
• MRD: Ph- immunofenotipo
-
Leucemia Mieloide Acuta
-
984-993 LEUCEMIE MIELOIDI
LAM con traslocazioni citogenetiche ricorrenti:9896/3 LAM con t(8;21)(q22;22), AML1(CBFα)/ETO M29866/3 LA Promielocitica [LAM con t(15;17)(q22;q21) e varianti, PML/RAR-α] M39871/3 LAM con ipereosinofilia midollare [inv(16)(p13;q22) o t(16;16), cbfb/myh11] M4eo9897/3 LAM con anomalie 11q23 (MLL)
LAM con displasia multilineare 9895/3 LAM con/senza precedente sindrome mielodisplastica9920/3 LAM e sindromi mielodisplastiche correlate a terapie agenti alchilanti, epipodofillotossine, altri tipi
LAM non altrimenti classificate9872/3 LAM scarsamente differenziata M09873/3 LAM senza maturazione M19874/3 LAM con maturazione M29866/3 LA promielocitica M39867/3 LA mielomonocitica M49891/3 LA monocitica M59840/3 LA eritroide M69910/3 LA megacariocitica M79870/3 LA basofilica9931/3 Panmielosi acuta con mielofibrosi
9805/3 Leucemie acute bifenotipiche
9860/3 Leucemia mieloide, NAS
9861/3 Leucemia mieloide acuta, NAS
Classificazione WHO 1997
-
Emocromo con formula leucocitaria (ematologo esperto in morfologia)
• Blasti > 20% condizione necessaria e sufficiente
Di solito si associa anemia, neutropenia, piastrinopenia, non sempre è
presente leucocitosi (se presente >10.000/µL)
Può essere anche l’unico esame se paziente molto anziano e/o frail, nel quale si
decide esclusivamente terapia di supporto
Diagnosi di LAM Su sangue periferico:
-
• Striscio + Mielogramma
valutazione morfologica e quantitativa del midollo al microscopio ottico
(ematologo esperto in morfologia) per valutare la percentuale e la morfologia dei
blasti e la riserva emopoietica
• Citofluorimetria cellule fenotipo immunologico:
CD34, CD13+, CD14+, CD33+ (markers di differenziazione della linea mieloide)
Il pannello viene allargato ad altri antigeni anche allo scopo di identificare i LAIP da utilizzare
nello studio della MRD
• BOM:
solo in caso di aspirato non informativo
Diagnosi di LMA
Su agoaspirato midollare:
-
LAM: Citogenetica e biologia molecolare
• Citogenetica: ricerca di traslocazioni specifiche
utili a definire la prognosi
• Biologia molecolare: mutazione di FLT3, NPM1
e mutazione biallelica di CEBPa (definizione del
rischio nella citogenetica normale secondo le
raccomandazioni ELN e NCCN)
• FISH in casi selezionati
-
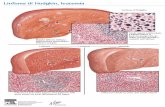
Leucemia promielocitica, FAB M3 APL
La traslocazione t(15;17) coinvolge il gene che codifica per il recettore nucleare a dell'acido retinoico RAR sul cromosoma 17 ed il gene PML (promielocitica) sul cromosoma 15 11 t(15;17)(q22;q11).
Fondamentale per la diagnosi e la terapia la
biologia molecolare con il monitoraggio del gene
ibrido PML-RARalpha, che va eseguito al termine
del consolidamento e poi ogni 2-3 mesi
-
LMA: Diagnostica avanzata
• Congelamento di cellule patologiche all’esordio
(utile per studi futuri)
• NGS (possibilità di sottogruppi sensibili a farmaci
in grado di inibire specifiche mutazioni)
-
LMA: Follow up
• RC: valutazione morfologica
• MRD: solo in studi clinici
• MRD: “mandatory” nella LAP
-
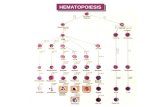
• Different clonal neoplastic disorders of hematopoietic stem cells
• Heterogeneous biologic and clinical characteristics
• “Rich marrow” (dysplastic, ineffective myelopoiesis due to excess of apoptosis) and “poor peripheral blood “ (variously combined cytopenias: anemia, leucopenia, thrombocytopenia)
• Low-to-high risk of leukemic transformation
• Very variable prognosis
Myelodysplastic Syndromes: a lot of directions
-
Myelodysplastic Syndromes
Increased apoptosis
Ineffective hemopoiesis
Lower-risk MDS: 75%
Apoptosis
Proliferation
-
Myelodysplastic Syndromes
Reduced apoptosis
Genetic evolution
Leukemic transformation
Higher-risk MDS: 25%
Proliferation
Apoptosis
-
Diagnosis and Evaluation
No specific clinical feature that distinguishes MDS from other causes of anemia (or other cytopenias)
Lab evaluation often prompted by signs or symptoms of the underlying cytopenias
– Fatigue, pallor, cardiac failure (anemia)– Infections (neutropenia)– Bleeding, ecchymoses, petechiae (thrombocytopenia)
-
Minimum work-up (1)
• Detailed patient’s history of transfusion need, professional toxic exposure and chemotherapic or radio-therapic treatments*, as well as severe co-morbidities
• Complete blood count, a peripheral blood smear examination with differential leukocyte count and a bone marrow aspiration with cytogenetics and morphologic evaluation, including Perls staining
• Bone marrow biopsy in order to assess marrow architecture, cellularity (hypoplastic MDS), fibrosis (primary myelofibrosis) and percentage of blasts
SIE, SIES and GITMO Guidelines, Santini et al. Leuk Res 2010* Secondary/Therapy-related MDS
-
• Serum erythropoietin determination in patients with symptomatic anaemia
• Iron status evaluation, i.e. serum ferritin and transferrin saturation in patients who are transfusion dependent or who start transfusion therapy
• DEB test in patients younger than 30 years who are possible candidates for high-dose chemotherapy or allogeneic HSCT, in order to exclude a Fanconi anaemia-associated MDS that is contraindicating chemotherapy
• HLA typing in patients eligible for HSCT, and those with an hypoplastic bone marrow (HLA-Dr15), in order to further support decision on immunosuppressive therapy
Minimum work-up (2)
SIE, SIES and GITMO Guidelines, Santini et al. Leuk Res 2010
-
Malcovati et al, European LeukemiaNet Guidelines, Blood 2013
B-2
* Prothrombin time
*
-
Malcovati et al, European LeukemiaNet Guidelines, Blood 2013
*
*
* and monocytes
-
301
530 529
0
100
200
300
400
500
Hb < 8 gr/dl Hb da 8 a 10 gr/dl Hb > 10 gr/dl
22% 39% 39%
FISM data: Cytopenias in 1361 MDS patients
232
339
786
0
100
200
300
400
500
600
700
800
100
17% 25% 58%
161213
371
573
0
100
200
300
400
500
600
2000
12% 16% 28% 44%
Anemia
Thrombocytopenia
Neutropenia
-
• Idiopathic
• Cytopenia/Dysplasia
• Undetermined
• Significance
• Might be MDS, but might not
• Needs follow-up, no treatment!
A definitive diagnosis
of MDS may be not
immediate!
ICUS / IDUS
-
Tefferi and Vardiman, N Engl J Med, 2009
E:%5CFebruary,%2024%20Tutorial%202004%5CTalocci5revmanResulting%20image.htmE:%5CFebruary,%2024%20Tutorial%202004%5CTalocci5revmanResulting%20image.htmhttp://www.google.it/url?sa=i&rct=j&q=&esrc=s&frm=1&source=images&cd=&cad=rja&uact=8&docid=ahOEwzu0pF5wOM&tbnid=wGdbYjo_1TB1CM:&ved=0CAUQjRw&url=http://imagebank.hematology.org/ImageBrowser.aspx?CategoryID=365&LevelID=1&ParentID=360&ei=jSh6U5XaCcneONnqgegK&bvm=bv.66917471,d.bGQ&psig=AFQjCNFwuGCXLB7FDi7ohYfgV6n4t8OPBw&ust=1400601008285388http://www.google.it/url?sa=i&rct=j&q=&esrc=s&frm=1&source=images&cd=&cad=rja&uact=8&docid=ahOEwzu0pF5wOM&tbnid=wGdbYjo_1TB1CM:&ved=0CAUQjRw&url=http://imagebank.hematology.org/ImageBrowser.aspx?CategoryID=365&LevelID=1&ParentID=360&ei=jSh6U5XaCcneONnqgegK&bvm=bv.66917471,d.bGQ&psig=AFQjCNFwuGCXLB7FDi7ohYfgV6n4t8OPBw&ust=1400601008285388
-
• It demonstrates the clonality of the disease, resolving problems of differential diagnosis
• It allows to identify specific genomic regions where genes involved in the pathogenesis of the disease are located
• It contributes to recognize specific biological and clinical entities
• It is probably the most important prognostic factor
• It may be helpful for monitoring the effects of therapies applied
Clinical relevance of detecting chromosomal abnormalities at diagnosis
-
Malcovati L, Educational Book, EHA 2012
-
Recurring chromosomal abnormalities in
t - MDS / t - AML
Normal
8%Balanced
4%
Other
12%
Abnl 5
22%
Abnl 7
30%
Both 5/7
24%
-
SingleDel(11q)-Y
Schanz et al, J Clin Oncol 2011
Prognostic relevance of cytogenetic abnormalities in MDS
-
FAB WHO• Not described Uni/Multilineage dysplasia • Not described MDS with isolated del(5q)
• RAEB-T (BM blasts 20-30%) > AML
• CMML > MDS/MPD
-
• del5q as unique chromosomal abnormality
• Macrocytic anaemia, slight leucopenia, normal to elevated platelet
• Small, hypolobated, mononuclear, spheronuclear megakaryocytes
• Predominantly middle-aged to older women
• < 15% blasts in blood and marrow
• Refractory anaemia, erythroid dysplasia/ hypoplasia, transfusion dependence
• Indolent course, 10–15% acute myeloid leukaemia, median survival > 5 years
• Interstitial, variable size 5q13-33 deletions (CDB: “common deleted band” 5q 31-32) in hematopoietic stem cells
• Marked hematological and cytogenetic response to lenalidomide
5q- “syndrome”: a distinct form of MDS in a subset of patients with isolated del 5q
Evidence suggests that haploinsufficiency of genes encompassed in or around the CDB
5q32–33 leads to the development of 5q– syndrome
..%5CFebruary,%2024%20Tutorial%202004%5CTalocci5revmanResulting%20image.htm..%5CFebruary,%2024%20Tutorial%202004%5CTalocci5revmanResulting%20image.htm
-
Disease complexity and heterogeneity in MDS with del(5q)
MDS del(5q)
• There is a general belief that MDS with del(5q) as an isolated cytogenetic abnormality has a favorable prognosis
• This is probably due to confusion about an old definition of the term “5q-syndrome”, that should be reserved only
to a distinct form of MDS in a subset of patients with isolated del 5q and well defined clinical and morphological
characteristics (see above)
• Today, there is increasing evidence that del(5q) MDS is heterogeneous with respect to clinical, pathological,
molecular and prognostic findings
Platelet count
Karyotype
complexity
Extend of
deletion Transfusion
status
Age/Sex
TP53
mutationsErythroid
hypoplasiaBM Blast count
WHO
morphology
-
The FAB had also already arbitrarily
categorized CMML into MDS-like and
MPD-like groups, using a white blood
count of 13x109/L as a cut-off to
differentiate the two entities.
Chronic Myelo-Monocytic Leukemia
-
Refractory anaemia with ring sideroblasts (RARS) and RARS with marked thrombocytosis (RARS-T):
provisional entity in the WHO 2008 classification characterized by high proportion of JAK2V617F and SF3B1 mutations
Cazzola et al, Blood, 2013
RARS
RARS-T
-
International Prognostic Scoring System (IPSS)
Punteggio RischioSopravvivenza
mediana(anni)
0 Basso 5,7
0,5-1,0 Intermedio-1 3,5
1,5-2,0 Intermedio-2 1,2
2,5 Alto 0,4
Modificata da Greenberg P, et al. Blood 1997;89:2079-2088.
* ANC
-
Effect of comorbidity on survival of MDS patients
Overall Survival Risk of Non-Leukemic Death
Della Porta et al, Haematologica 2009
-
Italian registry for MDS:
Presence of comorbidities (n = 388)
• CIRS, Cumulative Illness Rating Scale.
142
99
7770
0
20
40
60
80
100
120
140
160
Grade 0–2 n. 1 n. 2 n. > 2
20% 18%25%37%
Pa
tie
nts
, n
Comorbidities
63% with (at least one) comorbidities degree > 3 (CIRS)
-
5
12
19 18
3634
29
14
0
5
10
15
20
25
30
35
40
< 60 anni 61-70 71-80 > 80 anni
MDS indipendente MDS correlabile
22
5
149
1510
38
54
0
10
20
30
40
50
60
%
RA/RARS RCMD CMML RAEB
MDS indipenenti MDS correlabili
55
27
15
39
0
10
20
30
40
50
60
%
IPSS low-int1 IPSS int2-high
MDS indipendente MDS correlabile
Dati su 167 decessi in pazienti con SMD
-
Bejar, Haematologica 2014
Impact of mutations on survival of MDS patients
-
0 5 10 15 20 25 30 35 40Time from randomization (months)
0
10
20
30
40
50
60
70
80
90
100
Pe
rcen
tage s
urv
ivin
g
CCR
AZA
Difference in median OS was 9.4 months
24.4 months
15 months
50.8%
26.2%
100 200 300 400 500
1.0
0
0.25
0.50
0.75
0
0
Duration, months
Pro
po
rtio
n
su
rviv
ing
Non-chelated (n = 336)
Chelated (n = 264)
Lyons RM, et al. Blood. 2012;120:abstract 3800.
Fenaux et al, Blood 2011
Park et al, Blood 2008
Fenaux P, et al. Lancet Oncol. 2009;10:223-32.
Impact of novel treatments on survival of MDS patients
Erythropoietin
Chelation therapy
P < 0.0001 Lenalidomide
Azacitidine