Biologia Molecolare: Leucemie Mieloidi Acute
Transcript of Biologia Molecolare: Leucemie Mieloidi Acute

Biologia Molecolare: Leucemie Mieloidi Acute
Maria Teresa VosoDipartimento di Biomedicina e Prevenzione
Università Tor Vergata, Roma 20’

Name of Company
Research support
Employee Consultant Stockholder Speaker’s Bureau
Advisory Board
Other
Celgene/BMS x x x
Astellas x
Jazz x x x
Abbvie x
Disclosures

WHO classification of acute myeloid leukemia and related neoplasms
Arber et al., Blood 2016
*
* Defined by MDS-cytogenetics in about 30% of cases
~60-65%
~30%
~10%

AML-MRC
Cytogenetic abnormalities
Previous history of MDS or MDS/MPNDysplasia in >50% of cells in 2 or more BM lineages, in the absence of NPM1 or CEBPA mutations

Genetic heterogeneity of Acute Myeloid Leukemia
Dohner et al., Blood 2017

Adapted from Dohner H et al., Blood 2017
European LeukemiaNet (ELN) 2017: prognostic stratification
with FLT3-ITDlow

Impact of cytogenetics on survival
Analysis of 5,876 cases entered in MRC AML10, 12, and 15 trials
Grimwade D. et al., Blood. 2010*Excluding patients with t(15;17), t(8;21), inv(16), t(9;11), t(6;9), inv(3)/t(3;3). **Excluding patients with any other abnormalities listed previously.

• Targeted resequencing of 111 myeloid cancer genes (combined with cytogenetic profiles) in 1540 AML patients
• 5,236 driver mutations (i.e. fusion genes, copy number alterations, gene mutations) involving 77 loci
• 6 genes mutated in >10% patients; 13 genes 5-10% patients; 24 genes 2-5% patients; 37 genes <2% patients
Additional mutations by NGS
Adapted from Papaemmanuil E. et al., N Engl J Med. 2016
Genomic classification
Risk-adapted strategies
Therapeutic targets

NPM1/FLT3-ITD mutations
50-60% of NK-AML cases
One of the most frequently mutated gene in AML
Associated with good prognosis without concomitant mutation of FLT3-ITD or with FLT3-ITDlow
NPM1 represents an important prognostic indicator in AML
Pratcorona et al, Blood 2013
Overall Survival CIR
161 NPM1-mut pts, FLTD-ITDallelic ratio: high: >0.5
low: <0.5

Other mutations
Schnittger S. et al., Blood 2011
Mutations of RUNX1 present in 10–16% of AML RUNX1mut AML is a new provisional entity in the
revised WHO classification RUNX1 mutations are associated with adverse
overall survival and with disease progression
TP53 mutations present in 5–10% of AML Prognosically unfavourable, especially in
multi-hit state
Prochazka KT. et al., Haematologica 2019

“very favorable”
“favorable”
“intermediate”
“adverse”
“very adverse”
Patients with inv(16)/t(16;16) or biallelic
CEBPA mutations
Patients with TP53 mutations and a complex karyotype
Refinement of the 2017 ELN genetic risk stratification of AML
“favorable”
“intermediate”
“adverse”
ELN-2017
Adapted from Herold T. et al., Leukemia 2020
Refined ELN-2017Relapse-free survival
Overall survival

- PML-RARA: 24 hours - RUNX1-RUNX1T1, CBFB-MYH11, KMT2A, (Chr 5/7 FISH panel): 2–3 days- G-banding: 1 week
- FLT3 ITD, TKD, NPM1: 72 hrs - CEBPA: 1 week
What do we need from the labs
Immunophenotype (LAIP)
1. Arber DA, Erber HP. Am J Clin Pathol 2020;154:731–41;2. Döhner H, et al. Blood 2017;129:424–47
Prior to starting treatment
To plan post-remission therapy
CEBPA, RUNX1, ASXL1, TP53or extended gene panel
or whole genome sequence
AML-MRC

Impact of MRD in patients with AML in remission post-IC3
Identification of ≥ 0.1% MRD by multiparameter flow cytometry, or molecular methods is an important
prognostic marker that can help guide treatment (Tx) decisions
Short et al. JAMA Oncol 2020
Overall Survival Disease-free Survival
Dynamic Survival Prediction: Minimal/measurable Residual Disease (MRD)

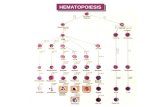
Preleukemic Leukemic
FLT3-ITDFLT3-TKDRASPTPN11KIT
DNMT3ATET2ASXL1IDH1/2SF3B1
PML/RARANPM1RUNX1-RUNX1T1CBFB-MYH11Other transloc.
SensitivePotentially unspecific
SpecificLost in 10-50%
SensitiveSpecific
Post-Onset Drivers
Suitability of MRD Detection Markers

QRT-PCR for PML/RARA
Cicconi et al., Leukemia 2016, Diverio et al, Blood 2008
>60% of patients tested +ve for PML/ RARA after induction therapy
Reduction of PML/RARA after induction was greater in patients receiving ATRA–CHT
PML/RARA levels at the time point of post-induction were not predictive of subsequent relapse
Kinetics of PML/RARA clearance in pts treated with ATRA-chemo vs ATRA-ATO
Diagnosis
Post-induction
Post III consolidation
PML/RARA +ve patients by QRT-PCR Cumulative Incidence of Relapse

MRD by RQ-PCR in PB after 2 Cycles of CHT
Ivey A et al., NEJM 2016
NPM1-mut in 2° post cons: higher risk of relapse at 3 years and lower rate of survival
BM MRD testing for NPM1-mutated AML does appear to be more sensitive than testing via PB
The presence of MRD in PB was highly informative among patients in morphologic CR
QRT-PCR for NPM1mut: PB better than BM

Log-reduction of transcripts predicts relapse in CBF-AML
• Upfront genetics and MRD determination in CBF-AML
• 198 patients
• QRT-PCR transcripts determination after first consolidation
• A less than 3-log MRD reduction or a level >0.1% was associated with a higher specific hazard of relapse
Jourdan et al., Blood 2013

Targeted NGS at diagnosis and after induction therapy (during CR)
Jongen-Lavrencic et al. NEJM 2018
Persistent mutations were detected in 51.4% of the patients
“DTA” mutations were most common
MRD monitoring by NGS

Kronke et al J Clin Oncol 2011Jongen-Lavrencic M, et al. N Engl J Med
MRD: NGS vs MFC or both?
MRD, assessed by cytofluorimetry (MFC) or molecular methods, including NGS, significantly predicts relapse
NGS has significant additive value to MFC

Normal-K AML at relapse
Greif et al, Clin Cancer Res 2018
Karyotype evolution:6/28 (21%)
Disease evolution at Relapse
Schmalbrok et al, Blood 2021
FLT3-ITD mutations

Markers Diagnosis Prognosis MRD Targeted Th.
PML-RARA x x x x
RUNX1/RUNXT1 x x x
CBF/MYH11 x x x
NPM1mut x x x
FLT3-ITD x x
FLT3-TKD x
CEBPAmut BA x
RUNX1 x x
BCR-ABL x x x x
TP53 x
ASXL1 x
t(9;11), inv(3), t(6;9), t(1;22)
x x
MDS-RC K x x
Clinical Role of Molecular Markers

WGS for AML diagnosis
Duncavage et al., NEJM 2021

Personalized Medicine in AML

Acknowledgements
M. Domenica DivonaEmiliano Fabiani
Giulia FalconiTiziana Ottone
Serena Travaglini
Giorgio ArceseFrancesco Buccisano
Maria Ilaria Del PrincipeLuca Maurillo
Raffaele PalmieriAdriano Venditti