UNIVERSITA’ DEGLI STUDI DI PADOVA Scuola di · PDF fileUNIVERSITA’ DEGLI STUDI DI...
Transcript of UNIVERSITA’ DEGLI STUDI DI PADOVA Scuola di · PDF fileUNIVERSITA’ DEGLI STUDI DI...
I GRAND ROUNDS DEL GIOVEDI’delle
Scuole di Specializzazione dell’Area Medica
UNIVERSITA’ DEGLI STUDI DI PADOVA
ScuoladiMedicinaeChirurgia
Cancer immunotherapy:the beginning of the end?
Direttore:Prof. PierFranco Conte
Relatori:Dott.ssa Alice MenichettiDott. Alberto Pavan
09 Giugno 2016Padova
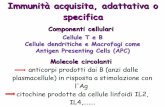
Immune System and Cancer
Cancer immune surveillance hypothesis: a process through which the immune system identifies and eliminates self-cells that have become transformed.
PRECLINICAL-Lymphocyte-deficient mice are highly susceptible to MCA (methylcholanthrene)-induced tumor development
EPIDEMIOLOGICAL-Recipients of a kidney, liver, heart, or lung transplant have an increased risk (incidence ratio of 2,1) for diverse cancers, compared with the general population
BIOLOGICAL-A strong lymphocytic infiltration has been reported to be associated with good clinical outcome in many different tumour types
V Shankaran et al, Nature 2001Vajdic CM et al, JAMA 2006
Tumor-Infiltrating-Lymphocyte
WH Fridman et al, Nature Reviews Cancer 2012Dieci MV et al, Annals of Oncology 2013
- Positive correlation between strong lymphocytic infiltration and outcome in several tumor types (melanoma, breast and ovarian cancer, head and neck carcinoma, oesophageal and colon cancer, bladder and prostatic cancer, lung cancer)
- The presence of TILs in residual disease after a neoadiuvant Chemotherapy is associated with better prognosis in TNBC patients
Strategy Pathway Mechanism
Negative Feedback Immune checkpoint(CTLA-4, PD-1)
Reduced T-cell proliferation, cytokine production and survival
Impaired antigen presentation
Defective antigen processing
Mutation or downregulation of tumor antigens or MHC genes, defects in antigen processing
Immunosuppressive tumour
microenvironment
Cytokines (TGF-β, IL-10, VEGF, etc.),
prostaglandinsRegulatory T reg
and MDSC
Reduced T-cell activationFavoured tumour outgrowthAngiogenesis
Apoptosis resistance FasL
Expression of anti-apoptotic molecules, downregulation and mutation of pro-apoptotic molecules
Tumor immune escape mechanisms
DM Pardoll, Nature Reviews Cancer 2012
Immune checkpoints
• Maintain self-tolerance• Modulate the duration and amplitude of
immune responses in peripheral tissues
The blockade of immune checkpoints unleashes the
antitumor immune response
CTLA-4 pathway
CTLA-4:•is expressed on activatedT-cells•counteracts the activity of T-cell co-stimulatory receptor CD28•downregulates early stages T-cell activation
Buchbinder EI et al, Am J Clin Oncol 2015
PD-1 pathway
PD-1•is expressed on activatedT-cells•regulates T-cell activation through binding to PD-L1 and 2•downregulates effector T-cell activation in peripheral tissue•hallmark of “exhausted” T-cells after high levels of stimulation
Pardoll DM, Nature 2012
CTLA-4 and PD-1: a comparison
CTLA-4Cytotoxic-T-Lymphocyte Antigen 4
Expression: T cells (CD8+, CD4+)
Ligand: CD80 and CD86 on APC
Regulates the amplitude of T-cell activation in lymphoid tissues
CTLA-4 blocking antibodies: IPILIMUMAB and TREMELIMUMAB
PD-1 Programmed Cell Death Protein 1
Expression: activated T cells, NK and B cells
Ligand: PDL1 and PDL2 on immune cells and non immune cells (including tumor cells)
Limits T cell activity within peripheral tissues
PD-1 blocking antibodies: NIVOLUMAB and PEMBROLIZUMABPD-L1 blocking antibodies: ATEZOLIZUMAB and DURVALUMAB
Clinical Case #1: V.I.
Physiological History-Male, aged 71-Smoker (30 pack years)-No family history of cancer-Retired; worked as an industrial worker for over 40 years
Medical History-Arterial hypertension
June 2010-Cough, no fever-Right chest parietal pain
1st Treatment:-Empirical antibiotic therapy
Chest Rx:-Suggestive for pleural empyema
August 2010SURGERY:-Right pleural decortication
Histological Examination-Epithelioid Mesothelioma
Clinical Case #1: V.I.
August-September 2010Multidisciplinary Evaluation:
18/08/10
08/09/10
29/09/10
NEOADIUVANT CTCarboplatin + Pemetrexed q3w
November 2010SURGERY:
-Right pleurectomy with
right lung decortication +
prosthetic emi-diaphragm
January 2011-December 2012-Regular follow-up: negative
Histological Examination-Localization of Mesothelioma
Clinical Case #1: V.I.
December 2012-CT scan: pleural PD PET-CT
January-May 2012Relapse Treatment Carboplatin + Gemcitabine for 5 cycles
June 2012-June 2013-Follow-up with CT scan: SD
June 2013-CT scan: lung PD
- CT-guided pleural biopsy
July 2014-Enrolled in Medimmune D4880C00003 II phase trial
Clinical Case #1: V.I.
September 2014-After 2nd administration Diarrhoea G1
1st Treatment:-Support-Loperamide- Persistence, no resolution within 10 days:
• Hospitalization Prednisone 1 mg/kg/die
October 2014-During steroid tapering Diarrhoea G2
• Hospitalization Prednisone 2 mg/kg/die
- No fever, no other symptoms- No microbiological findings on stool sample
- Abdominal Rx: no perforation, dilated bowel
R
2nd-3rd Line for Unresectable
Pleural Mesothelioma
Tremelimumab 10 mg/kg q4w
Placebo
October 2014-Rectal-sigmoidoscopy:
• Mucosal swelling• Fibrin membranes
Clinical Case #1: V.I.
November 2014-Acute abdominal pain
Rx: perforation
SURGERY:-Hartmann procedure: resection of 15 cm of left colon + sigma, cutaneous colostomy
- Physical deterioration, mental decline Best supportive care
End of November 2014 Death
Clinical Case #2: T.L.
Physiological History-Female, aged 31-No family history of cancer-Office worker
Medical History-In 2004: surgical removal of a compound nevus on the left calf
April 2008-Surgical removal of an ulcerated melanocytic lesion on the left calf
Histological Examination-Melanoma: Breslow 11 mm, Clark V (hypoderma)
- Sentinel Node Biopsy: negative
- Whole body CT scan: negativeSTAGE II C-T4b N0 M0
June 2008-June 2009Adiuvant Treatment High Dose IFN-γ
Clinical Case #2: T.L.
July 2009-July 2015-Regular follow-up: negative
July 2015-Surgical removal a subcutaneous node, next to the previous lesion
Histological Examination-Localization of Melanoma-B-RAF mut (V600E)
- Whole body CT scan: negative
September 2015-Enrolled in CHECKMate 238 phase III trial
q6w10 mg/kg
d1 d15 d22 d29
IPI P IPI P
q6w3 mg/kg
d1 d15 d22 d29
Nivo Nivo P Nivo
R
Complete Resected
Stage IIIb/c-IV Melanoma
Clinical Case #2: T.L.
December 2015-After 2nd cycle Diarrhoea G1
1st Treatment:-Support-Loperamide- Recurrence after 1 week:
• Prednisone 1 mg/kg/die
- Recurrence after 3 weeks:• Prednisone 2 mg/kg/die
January 2016-During steroid tapering Diarrhoea G2
• Hospitalization
- No fever, no other symptoms- No microbiological findings on stool sample
- Abdominal Rx: negative
Clinical Case #2: T.L.
January 2016-Steroid-resistant colitis Infliximab 5 mg/kg
Preliminary testing
QTferon Neg
Chest Rx Neg
HBV test Neg
Cardiological evaluation Neg
- Progressive resolution during hospitalization- No adverse effects from Infliximab
February-April 2016-Slow steroid tapering No recurrent episodes
March & May 2016-Drop out from the trial-Regular follow-up: negative
• Whole body CT scan: NED
Clinical Case #3: C.M.Physiological History-Male, aged 36-Exposed to second-hand smoke (father for over 30 years)-No family history of cancer-Work as a coach driver
Medical History-None
November 2014-Cough, mild dyspnoea
Bronchoscopy with biopsies:
Histological Examination-Squamous Cell Lung Cancer
Whole body CT scan:RSL nodule (11 cm) + right hilar adenopathy
January 2015Multidisciplinary Evaluation:
19/01/15
02/03/15
09/02/15
NEOADIUVANT CTCarboplatin + Gemcitabine q3w
Partial Response
April 2015- PET-CT scan: PD (lung + nodes)
May 2015- Starts Nivolumab 3 mg/kg q3w [compassionate]
Clinical Case #3: C.M.
Clinical Case #3: C.M.
1stdose
09/06/15
23/06/15
07/07/15
21/07/15
04/08/15
25/08/15
08/09/15
22/09/15
06/10/15
20/10/15
03/11/15
6thdose 11thdose
RevaluationCTscan
RevaluationCTscan
RevaluationCTscan
Clinical and radiological stability
June-November 2015
Clinical Case #3: C.M.
November 2015-Diarrhoea G2, persistent despite Loperamide
- Increased serum amylase and lipase
- Abdominal US CT scan Cholangio NMR: negative
Treatment-Fasting, PN-Antibiotic e.v.-Methylprednisolone 1 mg/kg/die
Clinical Case #3: C.M.
11/0
1/16
14/1
2/15
28/1
2/15
12thdose
13thdose
14thdose
December 2015-Resume Trial
Pneumonia G1-No fever, no symptoms-No CRP elevation-No microbiological findings on blood sample
Stable Disease, but…
Methylprednisolone 1 mg/kg/die
Clinical Case #3: C.M.
End of January 2016 End of February 2016
March-May 2016-Whole body CT scan: Stable Disease
Physiological History-Female, aged 44-Smoker (15 pack years)-No family history of cancer-Office worker
Medical History-None
October 2013-Abdominal pain-Decreased Hb (6,4 g/dL)
Clinical Case #4: P.S.
November 2013-Starts regular follow-up
SURGERY: Left nephrectomy + Lymphadenectomy
Histological Examination-Clear Cell Renal Carcinoma; Fuhrman G3
-Invading peri-renal fat;
STAGE III-T3a N0 M0
March 2015-Whole body CT scan: pulmonary micronodules Close Follow-up
Clinical Case #4: P.S.
June 2015-Whole body CT scan: increased pulmonary micronodules
July 2015-Enrolled in CHECKMate 214 phase III trial
R
Previously Untreated,
Advanced or Metastatic Renal Cell Carcinoma Sunitinib 50 mg/die for 4 weeks q6w
q3w for 4 cycles
IPI 1 mg/kg
+ Nivo 3 mg/kg
Nivo 3 mg/kg q2wUntil PD or tox
September 2015-Whole body CT scan after 4 cycles: Complete Response
Clinical Case #4: P.S.
October 2015-Malaise, fatigue-Fever (39,5°C)-No coughing, no dysuria, no other symptoms
Febrile Neutropenia-WBC 730/mL, N 200/mL
Anaemia G3-Hb 7,6 g/dL
Hepatic Toxicity G4-AST 932 U/L ALT 1180 U/L-gGT 366 U/L-Tot Bil 46,8 mmol/L (C. 35)-LDH 1736 U/L
Clinical Case #4: P.S.
First Measures
- Admitted to sterile room
Diagnostics (1)-Chest Rx-Blood and urinocolture-Oropharyngeal swab-Serology:
• HAV, HBV, HCV• CMV, EBV, HSV, VZV• Parvovirus B19
Empirical Treatment
- Antibiotics:• Piperacilline/Tazobactam• Amikacine
- Antifungal prophylaxis:• Fluconazole
- G-CSF- Methylprednisolone 2
mg/kg/die
NEGATIVE
- Support
Diagnostics (2)
Clinical Case #4: P.S.
- Blood smear:
- Bone marrow aspiration:
- Peripheral blood IFT:
- Bone marrow biopsy: Punctio Sicca
Clinical Case #4: P.S.
• Corticosteroid• G-CSF• Ig ev +
Cyclosporine• Ig ev
• Corticosteroid• G-CSF• Ig ev• ATG +
Cyclosporine + Methylprednisolone
Methylprednisolone 4 mg/kg/die
Clinical Case #4: P.S.
22-sep 20-oct 23-oct 29-oct 3-nov 9-nov 12-nov 14-nov 18-nov 26-nov 25-jan 15-feb 16-mar0
2
4
6
8
10
12
14
16
18
Methylprednisolone 2 mg/kg/die
Steroid taperingMethylprednisolone 4 mg/kg/die
Ig ev 400 mg/kg/die
Cyclosporine 2,5 mg/kg/die + steroid tapering
Neutrophil count n.v. 1,80-7,80 x10^9/LHepatotoxicity
Resolution
Clinical Case #4: P.S.
November 2015-Fever (>39°C), cough-Bilateral crackles-CRP 302 mg/L-PCT neg
Diagnostics-Blood and urinocolture-Serology:
• Aspergillus Ag• Beta-D-glucan
-Bronchoscopy + BAL
Positive
Aspergillus Flavus
December 2015-Starts Amphotericin-B-Transferred to Division of Infectious Diseases
Clinical Case #4: P.S.
22-sep 20-oct 23-oct 29-oct 3-nov 9-nov 12-nov 14-nov 18-nov 26-nov 25-jan 15-feb 16-mar0
2
4
6
8
10
12
14
16
18
Cyclosporine 0,3 mg/kg/die + tapering steroid
STOP Cyclosporine and steroid
February 2016-Whole body CT scan
April 2016-Whole body CT scan:
Complete Remission
Immune-Related Adverse Events (irAEs)
Unrestrained T-cell activation with immune checkpoints inhibitors translates into:
- antitumor responses- autoimmune breakthrough or irAEs
These toxicities require:-careful monitoring-specific management strategies
Reversible if treated promptly and appropriately
Immunosuppression using corticosteroid and other agents
Immune-Related Adverse Events (irAEs)
Anti CTLA-4-10% Hypophysitis and hypothyroidism
Anti PD-1-<10% Hypothyroidism
Anti CTLA-4-50% Rash and pruritus (trunk and extremities)
Anti PD-1-37% skin toxicity of all grades-6,5% dry mouth
Anti CTLA-4-30% Diarrhoea (only 10% G3-4)-5% Colitis G3-4
Anti PD-1-1-2% Diarrhoea G3-4
Anti CTLA-4-2.5% Hepatotoxicity G2-2% Hepatotoxicity G3-4
Anti PD-1-<5% Hepatotoxicity
Less frequent irAEs:•Pneumonitis•Asymptomatic pancreatitis•Hematologic syndromes•Ophthalmologic disorders•Renal insufficiency•Neurologic syndromes
Champiat S. et al, Annals of Oncology 2015Villadolid J. et al, Lung cancer diagnostics and treatments 2015
IrAEs: Kinetics of onset
Ipilimumab
Nivolumab
Villadolid J. et al, Lung cancer diagnostics and treatments 2015
IrAEs Management
How to stop immunosuppressive drugs?
Gradual corticosteroid tapering in at least 1 month
When to resume or terminate immunotherapy?
Temporary suspension Permanent discontinuation
- IrAEs stabilized < G1- Steroid dose reduced to < 10 mg/d
prednisone
- IrAEs G4- IrAEs G3 and recurring- IrAEs G2 not resolutive in 3 months
Immunotherapy dose reduction not recommended
No clear correlation between dose density and efficacy of immunecheckpoints inhibitors: Dose intensity not influenced by delaying immunotherapy
Ipilimumab: MDX 010-020 trial 676 subjects with advanced or metastatic pre-treated melanoma were randomized in this double-blind, phase III trial that compared:
- Ipilimumab 3 mg/kg + GP100 melanoma peptide vaccine
- Ipilimumab 3 mg/kg monotherapy
- GP 100 monotherapy
RESULTS
Hazard reduction for death of 32% and 34% respectively in the IPI+GP100 and IPI monotherapy groups compared with GP100 monotherapy group
No difference between the 2 groups receiving Ipilimumab
Hodi F. S. et al, N Engl J Med, 2010
IPI+GP100 vs GP100HR 0.68 (0.55-0.85; p=0.0004)
IPI vs GP100HR 0.66 (0.51-0.87; p=0.0026)
Median OS-IPI+GP100: 9.95 m -IPI: 10.12 m-GP100: 6.44 m
Primary endpoint: OS
Ipilimumab: CA 184-024 trial
Robert C. et al, N Engl J Med, 2011
IPI+DTIC median OS:11.2 m vs 9.1 m (p=0.0009)HR 0,72 (0,59-087)
502 subjects with metastatic untreated melanoma were randomized in this double-blind, phase III trial that compared:- Dacarbazina 850 mg/m2 + Ipilimumab 10 mg/kg (concurrent + maintenance)- Dacarbazina 850 mg/m2 + Placebo
Primary endpoint: OS
RESULTS
OS was significantly longer with Ipilimumab + Dacarbazine:- 1 yr survival rate 47% (vs 36)- 2 yrs survival rate 28% (vs 18)- 3 yrs survival rate 21% (vs 12)
Nivolumab: CHECKMATE-066
Robert C. et al, N Engl J Med, 2015
418 subjects with BRAF wild-type unresectable or metastatic untreated melanoma were randomized in this double blind, phase III trial that compared:
- Nivolumab (3 mg/kg, q2w)- Dacarbazine (1000 mg/m2, q3w)
Primary endpoint: OS
Nivolumab: CHECKMATE-017
Brahmer J. et al, N Engl J Med, 2015
272 subjects with advanced or metastatic squamous-cell non-small-cell lung cancer (NSCLC), progressed during or after 1st line platinum-based chemotherapy, were randomized in this open label, phase III trial that compared:
- Nivolumab (3 mg/kg, q2w)- Docetaxel (75 mg/m2, q3w)
Primary endpoint: OS
RESULTS
The risk of death was 41% lower with Nivolumab than with Docetaxel
Nivolumab: CHECKMATE-025
Motzer R.J. et al, N Engl J Med, 2015
821 subjects with advanced clear-cell renal-cell carcinoma, previously treated with one or two regimens of antiangiogenic therapy, were randomized in this open label, phase III trial that compared:
- Nivolumab (3 mg/kg, q2w)- Everolimus (10 mg/die)
Primary endpoint: OS
RESULTS
The risk of death was 27% lower with Nivolumab than with Everolimus
Pembrolizumab: Keynote-006834 subjects with advanced melanoma, who received no more than one previous systemic therapy, were randomized in this open label, phase III trial that compared:
- Pembrolizumab (10 mg/kg, q2w)- Pembrolizumab (10 mg/kg, q3w)- Ipilimumab (3 mg/kg, q3w)
Primary endpoint: OS and PFS
Robert C. et al, N Engl J Med, 2015
RESULTSHazard reduction for death of 37% and 31% respectively in the Pembrolizumab q2w and Pembrolizumab q3w groups compared with Ipilimumab group.
No difference between the 2 groups receiving Pembrolizumab
Future Directions: CHECKMATE-067
Larkin J. et al, N Engl J Med, 2015
945 subjects with unresectable previously untreated stage III or IV melanoma were randomized in this double blind, phase III trial that compared:
- Nivolumab (3 mg/kg, q2w)- Ipilimumab (3 mg/kg, q3w)- Nivolumab (1 mg/kg, q3w) plus Ipilimumab (1 mg/kg q3w)
Primary endpoint: OS and PFS
IrAEs and Effects on Survival
IrAEsG1-2 G3 G4 Total
47 % 31 % 7 % 85 %
Single centre retrospective analysis on 298 patients with melanoma treated with Ipilimumab 3 mg/kg q3w showed:
Most common IrAE: diarrhoea (14%)
Neither the occurrence of IrAEs nor the use of systemic corticosteroids influenced OS
Horvat Troy Z. et al, JCO 2015
IrAEs and Effects on SurvivalMulticentre retrospective analysis on 576 patients with advanced melanoma treated with Nivolumab 3 mg/kg q2w showed:
The use of systemic corticosteroids impacts neither Response Rate nor Median time to Response
Weber J.S. et al, JCO 2015 (suppl; abstr)
Total IrAEs: 49%
G3-4 IrAEs: 10%
Take Home Messages
- Immunologic-checkpoint inhibition targeting CTLA-4 and PD-1 has dramatically improved the care of patients with many advanced malignancies
- Treatment is associated with typically transient IrAEs, that have a completely different underlying mechanism compared to toxicities observed with chemotherapy
- Rapid identification of IrAEs and systemic immunosuppression can improve outcomes without compromising the efficacy of immune-checkpoint inhibition
- The clinical team have to be educated and aware of these potential toxicities if promptly recognized, they’re almost always reversible