Impact of Inherited Polymorphisms in Glutathione S ... · mary of patients’ characteristics,...
Transcript of Impact of Inherited Polymorphisms in Glutathione S ... · mary of patients’ characteristics,...

Vol. 7, 703-709, August 1998 Cancer Epidemiology, Biomarkers & Prevention 703
Impact of Inherited Polymorphisms in Glutathione S-Transferase M 1,
Microsomal Epoxide Hydrolase, Cytochrome P450 Enzymes on DNA,
and Blood Protein Adducts of Benzo(a)pyrene-diolepoxide1
Roberta Pastorelli,2 Marco Guanci, Annalisa Cern,Eva Negri, Carlo La Vecchia, Franco Fumagaffi,Maurizio Mezzetti, Roberto Cappelli,
Tiziana Pamgalli, Roberto Fanelli, and Luisa Airoldi
Department of Environmental Health Sciences [R. P., M. G., A. C., R. F.,L. A.] and Laboratory of General Epidemiology [E. N., C. L. V.], Istituto di
Ricerche Farmacologiche Mario Negri, 20157 Milan; and Division of Thoracic
Surgery, European Institute of Oncology, 20100 Milan [F. F., M. M., R. C.,
T. P.], Italy
Abstract
The benzo(a)pyrene (BaP) metabolite benzo(a)pyrene-diolepoxide (BPDE) is strongly implicated as a causativeagent of lung cancer. To assess the risk of exposure toBaP, we made a combined analysis of levels of BPDEadducts to hemoglobin (Hb), serum albumin (SA), and
lymphocyte DNA in 44 patients with incident lung cancer,as a prototype of a population mainly exposed to tobacco-derived BaP. We also investigated whether geneticpolymorphisms of cytochrome P4SOIA1 (CYPIA1),microsomal epoxide hydrolase (mEH), and glutathioneS-transferase Ml (GSTM1), which are involved in BaPmetabolism, can be determinants of adduct formation.
BPDE-Hb, BPDE-SA, and BPDE-DNA adducts werequantified as BaP tetrols released from hydrolysis ofmacromolecules and measured by high-resolution gas
chromatography-negative ion chemical ionization-massspectrometry to achieve high specificity and sensitivity.Individuals with detectable Hb adducts were positive forSA adducts but not vice versa, suggesting that BPDE-Hbadducts are less informative indicators of BaP exposure.
Using PCR methods on DNA, we characterizedGSTMJ deletion, CYPIAJ MspI and exon 7 valinevariants, and mEH polymorphisms at amino acidpositions 113 (EH3) and 139 (EH4).
Levels of BPDE adducts were no different among
CYPIAJ, mEH, and GSTMJ genotypes. However,individuals with measurable BPDE-SA adducts wereCYPIAJ variant carriers more frequently (P = 0.03).There was a slightly higher percentage of DNA detectableadducts in subjects with CYPIAJ exon 7 valine
Received I 2/23/97; revised 5/14/98; accepted 6/1/98.
The costs of publication of this article were defrayed in part by the payment of
page charges. This article must therefore be hereby marked advertisement inaccordance with 18 U.S.C. Section 1734 solely to indicate this fact.I This work was supported by the Italian National Research Council (Special
Project Applicazioni Cliniche della Ricerca Oncologica, Molecular Epidemiology
Program) and by the “Europe Against Cancer Program” of the Commission of the
European Community.
2 To whom requests for reprints should be addressed, at Istituto di Ricerche
Farmacologiche Mario Negri, Via Eritrea 62, 20157 Milan, Italy.
polymorphism. When subjects were classified by bothpolymorphisms on the mEH gene, those with two slowalleles (EH3 homozygous mutated) and no fast alleles(EH4 homozygous wild type) had a lower frequency ofBPDE-SA adducts and no DNA adducts (P 0.06).
These results are based on a small number ofobservations thus far, but this exploratory study suggeststhat CYPIAJ and mEH variants might have an impact onBPDE exposure markers such as BPDE-SA adducts.Chemical specificity in adduct measurements is importantto identify the biomarkers that reflect BaP exposure moreaccurately.
Introduction
BaP,3 a representative of the class of pulmonary carcinogensknown as PAHs, is an ubiquitous pollutant, found in automobile
exhaust, food, occupational settings, contaminated air, and to-bacco smoke. Thus, human exposure to this chemical is wide-spread and very likely related to overall lung cancer risk (1).
To identify quantitative indicators of human exposure tothis carcinogen, work has focused widely on monitoring PAHadducts in relation to BaP exposure and bioactivation in hu-mans. High levels of PAH-DNA adducts in human blood cells
and PAH albumin adducts have been associated with highambient levels of PAH, including BaP (2-4). One study re-ported a significantly higher level of PAH-DNA in lung cancer
cases than in controls, given similar current smoking patterns(5).
Within the p.53 tumor suppressor gene, the BaP ultimate
carcinogenic metabolite BPDE [(±) r-7, t-8-dihydroxy-t-9,
:-lO-epoxy-7,8,9,l0-tetrahydrobenzo(a)pyrene] preferentiallymodifies the guanine residue in the same mutational hot spots
as those in human lung cancer (6).
The conversion of BaP into DNA and protein-reactiveBPDE is dependent on a cascade of biotransformations, includ-ing BaP oxidation by CYPIAJ into benzo(a)pyrene-7,8-oxide,hydration by the mEH into benzo(a)pyrene-7,8-dihydrodiol,and a final P450-dependent oxidation step giving rise to thehighly carcinogenic BPDE (7). However, intermediate metab-olites and BPDE itself can be detoxified through differentpathways like conjugation with glutathione, catalyzed by theGST superfamily, which includes the isoenzyme GSTM1 (7).
Because the genes encoding the enzymes mentioned have
been found to be polymorphic in the human population, variousstudies have tried to relate the metabolic genotype to PAH-
3 The abbreviations used are: BaP, benzo(a)pyrene: PAH, polycyclic aromatic
hydrocarbon; BPDE, bcnzo(a)pyrene-diolepoxide: CYPIAI, cytochrome
P45OIA1 ; mEH, microsomal epoxide hydrolase; GST, glutathione S-transferase;Hb, hemoglobin; SA, serum albumin; BPT, BaP tetrols.
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

7()4 BPDE Adducts and Metabolic Polymorphisms
induced cancer risk. The GSTMJ gene codes for the detoxifi-
cation enzyme GSTMI and is deleted in -50% of the Cauca-sian population. The inherited absence of the GSTMJ gene (the
GSTMI null genotype) has been associated with a higher risk of
lung cancer (8-11).A mutation in the 3’-noncoding region of the CYPIAJ
gene, creating a new MspI cleavage site (ml), was overrepre-sented among lung cancer patients in Japan ( 1 2). The existenceof a link between this polymorphism and lung cancer is stilldebated in the Caucasian population, perhaps on account of the
considerably lower frequency of the variant allele among Cau-casians (13-15).
Conflicting results for a role of CYPIA] polymorphism inenhanced susceptibility to PAH carcinogenesis have also been
reported for the mutation in the catalytic region (exon 7) of thegene, closely linked to the MspI variant. The A-*G transition
creates an allelic variant (m2) with an associated amino acidsubstitution of Val-462 for Ile-462, resulting in enhanced en-
zymatic activity ( 16, 17). This polymorphism has been associ-ated with lung cancer in Japanese populations but not clearly inCaucasians, who have a much lower frequency of the mutanttrait (14, 18, 19).
Two point mutations have been described in the humanmEH gene, affecting enzyme activity: one, at amino acid po-
sition 1 13 in exon 3, changes tyrosine residue to histidine
(His-l 13), reducing the enzyme activity by at least 50%; an-other, at amino acid position 139 in exon 4, changes histidineresidue to arginine (Arg-139), producing an enzyme with ac-
tivity that is increased by at least 25% (20).The low-activity His-l 13 allele was associated with an
increased risk of hepatocellular carcinoma, presumably becauseof a reduction in the ability to detoxify aflatoxin B 1 (21). Todate, there are few reports relating mutant alleles of mEH withparticular cancer risk (22, 23), including PAH-induced cancer,although mEH is an important control point for directing thepathway of BaP detoxification and/or activation.
The question of whether metabolic polymorphisms act as
modifiers of exposure biomarkers is currently being widelyinvestigated. The GSTMJ null genotype has been associatedwith higher PAH-DNA adduct levels in lung tissue but not inlymphocytes (24, 25). PAH-DNA adduct levels in peripheral
WBCs may depend, in part, on particular GSTMJ and CYPIAJ
genotypes (26, 27), although negative results have been re-ported as well (24, 28). Thus, the relationship between markersof PAH exposure and markers of metabolic susceptibility is still
unclear.The controversial results might depend partly on differ-
ences in the analytical sensitivity and specificity of adduct
detection by immunological methods and 32P-postlabeling as-say, in which the exact chemical species responsible is not
identified. The lack of chemical specificity in adduct measure-ments might hinder the identification of any association with
specific metabolic polymorphism.Recently, we quantified BPDE-Hb adducts in a population
exposed to low levels of BaP, mainly from traffic exhaust (29),
using a gas chromatography-mass spectrometry method thatwas highly sensitive and specific for BPDE.
In this preliminary investigation, we applied the samemethod for the measurement of a battery of biomarkers, such as
BPDE adducts to Hb, to SA, and to lymphocyte DNA in agroup of lung cancer smoker patients as a prototype of a
population mainly exposed to tobacco-smoke-derived BaP. Wealso investigated the relative contribution of inherited meta-bolic capabilities (CYPIAJ, nzEH, and GSTMJ) on adduct pro-
file.
Table I Demographic characteristics o f lung cancer patients
Characteristic Value
Total no. of patients 44
% male patients 100
Age, mean (SD) 60 (8.3)
% smokers 100
Cigarettes/day. mean (SD) 29.7 (1.77)
Pack-years, mean (SD) 63.2 (4.7)
Histological classification (%)
Adenoearcinoma 36.4
Squamous cell 27.3
Small cell 9.1
Large cell 6.8
Other 20.4
Materials and Methods
Patients and Sampling. Forty-four male Caucasian patientswith incident, histologically confirmed lung cancer were en-
rolled at the time of their first admission to the EuropeanInstitute of Oncology in Milan between 1995 and 1997. Allwere still living their own lifestyle (all current smokers) and
had not yet had any pharmacological treatment.
A structured questionnaire was administered by trainedinterviewers, including information on occupational, dietary,
and detailed smoking histories. As an indication of cumulative
smoking exposure, pack-years were computed as the averagenumber of packs smoked per day multiplied by years of smok-
ing. The family history of cancer was also recorded. A sum-mary of patients’ characteristics, including histological classi-
fication, is presented in Table 1.After giving informed consent, each subject donated
40-50 ml of blood, which was collected in heparmnized tubes.Plasma, RBCs, and lymphocytes were separated by the Ficoll-Paque method (Pharmacia Biotech, Cologno Monzese, Italy)
within 4 h of sampling. Pelleted cells and plasma were stored
at -80#{176}C.
Isolation of DNA and Proteins. DNA was extracted from
frozen lymphocytes using the procedure described by Wu et a!.
(30), which requires no organic solvent extraction. Briefly, eachlymphocyte pellet was resuspended in 3.5 ml of lysis buffer
[400 msi NaCl, 100 msi Tris-HC1 (pH 8), 5 msi EDTA, 0.2%SDS, 20 j.�g/ml RNase A, and 500 �.tg/ml proteinase K) andplaced in a 10-cm culture dish at 37#{176}Covernight. After diges-
tion, an equal volume of isopropanol was added to each plateand gently mixed until the white DNA precipitate was seen atthe bottom of the dish. The dishes were then left undisturbed for2 h at room temperature. Because the DNA precipitate adheres
to the plastic dishes, the supernatant was poured off, and the
DNA was washed with ice-cold 70% ethanol. Air-dried DNAwas then dissolved in distilled water by incubation at 37#{176}Cfor2 h.
Albumin was isolated from plasma by addition of satu-rated ammonium sulfate (final concentration, 50%). After re-
moval of globulins by centrifugation, albumin was precipitatedfrom the supernatant by acidification with 1 M acetic acid (31).Albumin was redissolved in distilled water, and the protein
concentration was determined by Bio-Rad protein assay (Bio-Rad, Segrate Milanese, Italy).
Packed RBCs were lysed with 2 volumes of distilled waterand centrifuged to remove cell membranes. Hb concentrationwas measured by Drabkin’s method (Drabkin’s kit; Sigma,
Milan, Italy).
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

b
Fig. 1. Individual distribution of BPDE-Hb adducts
(a), BPDE-SA adducts (b), and BPDE-DNA adducts(c). Each sample was run in duplicate. Data points,
average values. Samples with undetectable adducts are
grouped (bottom). The limits of sensitivity were �0.05
fmol BPT/mg protein and � I .4 adducts/l09 nucleo-
tides.
a3
2.52
:� 0.4500)0Ea)
0
EI-ILc#{252}0.15
0.05 -� ________
0
C
(1)a)
�0
0a)0
C
a)0
Cl)
0
�0‘DCa
IL0�1
00
0
0
0
0
B
12-
8-
4-
1.4
�0
0.05i ________acticri�c
0
Cancer Epidemiology, Biomarkers & Prevention 705
BPDE Adducts Analysis. BPDE adducts to Hb, SA, and DNAwere measured essentially as described by Pastorelli et a!. (29).
Briefly, BPDE adducts were analyzed as BPT released fromDNA (200 ,Lg) and proteins (100 mg) after acid hydrolysis of
the macromolecules (0.3 N HC1 for 60 mm at 80#{176}C).DNAhydrolysates did not require any Extrelut purification and werebrought to neutral pH and directly loaded onto immunoaffinity
columns containing the 8E1 1 monoclonal antibody developed
by Santella et a!. (32). BPT were quantitated by high-resolutiongas chromatography-negative ion chemical ionization-mass
spectrometry with selected ion recording, using the stable iso-tope dilution technique (29).
Determination of Genetic Polymorphisms. All genotypeswere determined after gene amplification using PCR. Primerswere obtained from Duotech (Milan, Italy). PCRs were per-formed in the Hybaid Thermocycler (Celbio Srl, Milan, Italy)
using Taq DNA polymerase from Promega (M-Medical Sri,Florence, Italy) and dNTP solutions from Epicentre Technolo-gies (Societ#{224}Prodotti Antibiotici SpA, Milan, Italy).
GSTMJ deficiency was detected as described by Bell et a!.(33). /3-Globin was coamplified with GSTMJ as internal stand-
ard. mEH and CYPIA] polymorphisms were characterized by
RFLP after PCR. All of the restriction enzymes used wereobtained from New England Biolabs (Celbio Srl, Milan, Italy).
The tyrosine-histidine polymorphism of EH gene at amino
acid 1 13 in exon 3 (EH3) was analyzed by PCR amplificationwith the primers EPO1 (5’-GATCGATAAGTFCCGTT-TCACC) and EPO2 (5’-ATClTAGTCTTGAAGTGAGGAT),with a base change in primer EPO2 (underlined) to generate an
EcoRV restriction enzyme site for samples with the Tyr-l 13
allele only, according to Smith and Harrison (34).The histidine-arginine polymorphism at amino acid 139 of
mEH gene in exon 4 (EH4) was analyzed by PCR-RFLP using
the restriction enzyme RsaI, as described by Hassett et a!. (20).The T-sC mutation (ml) in the 3’-flanking region of CYPIAJ
was detected by PCR-RFLP analysis using the enzyme MspI
(1 8). The CYPIAJ IleNal replacement (m2) was detected by theimproved genotyping method reported by Cascorbi et a!. (18),
using the BsrDI-RFLP analysis.
Statistical Methods. The correlations between age, tumor his-tology, smoking habits, and adduct profiles were tested with theSpearman rank-order correlation. To compute mean adduct
C
E
0a)E
0E
I-ILm 0.15-
values, patients with unmeasurable levels were considered as
having half the minimum detectable value.Differences in adduct levels between genotype categories
were tested with the Wilcoxon rank-sum test (two categories)
and Kruskal-Wallis test (more than two categories).Fisher’s exact test was used to test the association between
genotypes and adduct frequency dichotomized in undetectable
and detectable. All tests were computed using SAS software
(35).
Results
Individual adduct levels in the 44 patients are presented in Fig.
1, in which Hb and SA adducts are expressed as fmol BPTreleased/mg protein hydrolyzed (Fig. 1, a and b, respectively).DNA adducts are shown as number of adducts/109 nucleotides(Fig. lc).
The limit of sensitivity for the detection of BPT was
�0.05 fmol/mg in human proteins, and in DNA, it was � 1.4
adducts/109 nucleotides.BPDE-Hb adducts were detectable in six subjects (13.6%)
with an overall median level of 0.025 fmol BPT/mg Hb.BPDE-SA adducts were measurable in 24 patients (56.8%;
median, 0. 1 1 fmol BPT/mg SA). BPDE-DNA adducts weredetectable in 18 (38.6%; median 0.7 adducts/l09 nucleotides).
When adduct levels were classified as detectable or unde-
tectable, the presence of Hb adducts was significantly associ-ated with the presence of SA adducts (P 0.029; Fisher’s exacttest). No associations were found with BPDE adducts to DNA.
There was a correlation between number of cigarettes
smoked daily and DNA adducts (r = 0.34, P = 0.02). Cumu-lative smoking, expressed as pack-years, was associated with
the DNA adduct level (r = 0.3, P = 0.05). No further associ-ations were found.
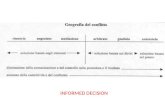
The distribution of the genotypes is shown in Fig. 2.
Twenty-three patients (52.3%) were GSTMJ null genotype,which results from the total absence of the gene.
Absence of the MspI site in both alleles, representing thehomozygous wild-type genotype (wtl/wtl), was seen in 38patients (86.4%), and the remaining 6 (13.6%) were heterozy-
gous (wtl/ml). Point mutational Ile-Val polymorphism (m2) inthe exon 7 of CYPIA] gene was found as a heterozygousconformation (wt2/m2) in three patients (6.8%), whereas the
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

C523 (�
� (21D
wti/wti � (3�j
wti/mi �i.6 ��?)CO (0)�
ml
GSTM1
CYPIA1 -
m EH -
a p by Wilcoxon rank-sum test.
/‘ Only one person.
Co (0�
C 5#{176}(2��
El 25 (liD
C25�D
� (27D
�.3 (l�
C2.3�Dmt/mt
706 BPDE Adducts and Metabolic Polymorphisms
For this preliminary investigation, we selected a group of lung
cancer patients who had a long history of smoking and were
GENOTYPE % of group (n)
mi/mi
wtVw�
m2 wt2Im2
EH 3
m2/m2
wUwt
wt/mt
mt/mt
wU�
EH4 #{149}� wt/mt
Fig. 2. Percentages of genotypes in lung cancer patients. Numbers in parenthe-
ses. numbers of patients.
rest were homozygous wild-type genotype (wt2/wt2). The pres-ence of one copy of the exon 7 variant polymorphism (m2) wassignificantly associated with the MspI polymorphism (ml; P
0.001, Fisher’s exact test, two-tailed). Because mutated allelesml and m2 are rare in the Caucasian population, no homozy-gous carriers were found in our group.
The EH3 polymorphism on rnEH gene was detected in50% ofthe population studied, with 25% being homozygous for
the mutated allele and 25% being heterozygous. Twenty-twowere genotyped as homozygous wild type (50%).
The majority of the subjects (61 .4%) were classified as
homozygous wild type for the EH4 polymorphism on mEH
gene. There were 16 heterozygous carriers (36.3%), and only 1(2.3%) had the homozygous mutated allele.
Table 2 shows the mean levels of BPDE adducts accordingto each genotype. The GSTMI genotype did not have any effecton BPDE-SA and DNA adducts. BPDE-Hb adducts werehigher in the GSTMI null group than in the GSTMJ positivegenotype, but the difference was not significant. Slightly higherlevels of Hb adducts were also observed in the homozygouswild type for each CYPIAJ variant (wtl/wtl and wt2/wt2)
Table 2 Mean adduc t levels in relation to genotype
BPDE-Hb adducts, BPDE-SA adducts, BPDE-DNA
Genotypefmol BPT/mg
protein
Mean (SE) pa
fmol BPT/mgprotein
Mean (SE) pa
adducts, noJlO’
nucleotides
Mean (SE) pa
GSTMI
Null 0.16 (0.10) 0.15 (0.03) 2.79 (0.56)
Positive 0.04 (0.0 1 ) 0. 1 2 0. 16 (0.03) 0.94 2.53 (0.78) 0.54
CYP1AI
wtl/wtl 0.1 1 (0.06) 0.14 (0.02) 2.46(0.44)
wtl/ml 0.05 (0.03) 0.84 0.23 (0.04) 0.07 3.99 (1.96) 0.45
ui2.Mt2 0.10 (0.06) 0.15 (0.02) 2.60 (0.47)
wt2Jm2 �0.05 0.48 0.28 (0.05) 0.08 3.57 (1.76) 0.44
EH3
wi/wi 0.04 (0.01) 0.18 (0.03) 3.05 (0.67)
we/tn: 0.04 (0.01) 0.16 (0.04) 1.68 (0.53)
mt/mt 0.27 (0.22) 0.75 0.09 (0.02) 0. 1 8 2.89 ( I .05) 0.47
EH4wI/st�t 0. I 3 (0.09) 0. 16 (0.03) 2.3 1 (0.44)
wt/m, 0.05 (0.18) 0.77 0.15 (0.03) 0.68 3.01 (0.99) 0.52
mt/tnt” �0.05 �0.05 6.9
compared to the heterozygous conformation (wtl/ml and w12/
m2). Increased levels of SA and DNA adducts found in the
presence of each variant were not significantly associated with
the heterozygous genotypes.No significant influence on Hb, SA, and DNA adducts
emerged with the presence of at least one mutated allele forEH3 and EH4 polymorphisms.
The presence of adducts was then divided into positive andundetectable. The frequency of detectable adducts in relation to
each genotype is reported in Fig. 3. Individuals with measurableHb and DNA adducts were more frequently GSTMJ null gen-
otype (Fig. 3A), but this tendency was not significant.
We classified the patients by CYPIAI polymorphisms inthree groups because the three who had the rare m2 polymor-
phism were a subset of those with the rare ml variant (Fig. 3B).
When detectable adducts were analyzed in relation to these
genotypes, the percentage of positive SA adducts was higheramong the heterozygous carriers than the wild type. A signif-icant association (P 0.03) was only found in SA adductswhen subjects with at least one variant were grouped together
and compared to those with no mutation on the gene. A non-significant doubling of detectable DNA adducts (66%) wasobserved in the presence of the m2 variant compared to thewild-type (36.8%) and ml mutated allele (33%) conformations.
Patients homozygous and heterozygous for EH3 variant
tended to have fewer detectable adducts to SA and DNA thanthose who were wild type (Fig. 3C), but this difference was notsignificant. The EH4 genotype was not associated with adduct
frequency (Fig. 3D).
Interestingly, after classification of subjects by both mEH
gene polymorphisms (EH3 and EH4), the six who had twomutated alleles on EH3 and no mutation on EH4 showed nodetectable DNA adducts and a lower frequency of detectableSA adducts than those presenting the remaining haplotypecombinations, as shown in Fig. 4 (P = 0.06 and P 0.3).
Discussion
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

1000 GSTM1 + [21] AU GSTM1 - [23]
(12)
(10)
� #{149} � r7�IBPDE-Hb BPDE-SA BPDE-DNA
60
40
100�
�- 80
U) 600
‘D‘DCa 40a)
.0Ca0a)a)
0�
a� l00�>�
I 80Cl) 600
VVCa 40a)
.0Ca� 20a)
0
20
0
C
BPDE-Hb BPDE-SA BPDE-DNA
E1 EH3 wt/wt [22]
. EH3 sit/mt + mt/mt [22]
(3) (3)
D
(14)
(10)
0 EH4 wI/wI (27]
U EH4 mt/mt+wt/mt (17]
(4) (2)
r-�BPDE-Hb BPDE-SA BPDE-Hb BPDE-SA BPDE-DNA
Cancer Epidemiology, Biomarkers & Prevention 707
100
I 80-
U) 60-0
�0�0Ca 40-a)
.0Ca0a,a)
0�
Fig. 3. Frequency of detectable adducts in relation to GSTMI genotype (A). CYPIA I genotype (B). EH3 genotype (C). and EH4 genotype ID). GSTMJ + , homozygous
positive and heterozygous genotypes; GSTMI-, homozygous null genotype; CYP/Al ml, MspI mutated allele: CYPIAJ ,,i2, exon 7 mutated allele: EH3 ,nt, mEH exon
3 mutated allele: EH4 mt mEH exon 4 mutated allele. Numbers in brackets, total numbers of subjects carrying each genotype: numbers in parentheses. numbers of subjects
with detectable adducts. *, P = 0.03, Fisher’s exact test, two-tailed, no mutation versus at least one mutated allele. None of the other differences were significant.
still smokers at the time of blood sampling, thus representing aprototype of subjects heavily exposed to the tobacco carcinogen
BaP. Neither occupational nor dietary BaP exposure was elic-ited by the questionnaire.
A unique aspect of our approach is the use of a highlyspecific method based on BPT released from hydrolysis of the
macromolecules and measured by high-resolution gas chroma-tography-negative ion chemical ionization-mass spectrometry,which achieves high sensitivity with a detection limit of 1.4
adducts/109 nucleotides and 0.05 fmol BPT/mg protein.This is the first comparative analysis of multiple dosime-
ters such as BPDE adducts to Hb, SA, and DNA in the samepopulation.
Our method found lower levels of BPDE adducts to pro-teins and DNA than those measured by other authors in smok-
ers (27, 36-38). This difference may be due to the fact that theimmunoassay techniques used by these authors measured sev-
eral types of PAH adducts due to cross-reactivity of the anti-body used.
The BPDE-Hb adducts levels we found were lower, but
comparable to those recently reported in smokers using a gaschromatography-mass spectrometry approach (39).
The percentage of individuals with detectable BPDE-Hbadducts was lower than that of individuals with measurable SAadducts. Individuals presenting Hb adducts were positive for
SA adducts but not vice versa, suggesting that BPDE-Hb ad-
ducts might be less informative than expected as a marker ofinternal dose.
Several studies report that PAH-DNA adducts in leuko-
cytes are associated with cigarette smoking and decline afterstopping smoking, (40) but the structure of the adducts has
never been reported. Here, we have shown that a significantassociation exist between BPDE-DNA adduct levels in lym-phocytes and cigarettes/day as well as pack-years.
The lack of correlation between blood proteins and DNAadducts in the same subject might be due to difierences inkinetics of these biomarkers (41).
The level of BPDE adducts is expected to be affected notonly by the exposure dose of BaP but also by metabolic poly-
morphism of the enzymes involved in its metabolism.
In our study, the GSTMJ genotype did not have anysignificant effect on BPDE adducts formation, possibly due tothe small sample size, but individuals with detectable Hb andDNA adducts were more frequently GSTMJ null genotype.
Conflicting results are reported on how the polymorphicCYPIAJ, the key enzyme in activation of many carcinogens,affects lymphocyte DNA adducts.
Shields et a!. (24) showed no correlation between PAH-DNA adduct levels and CYPIAJ in] variant in lung cancer
patients. Similarly, Hemminki et a!. (42) observed only a bor-
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

>�0Ca)
0’a)
U)
0
VVCaa)
.0Ca0a)a)
0
1 00
80
60�
40’
20’
0BPDE-Hb BPDE-SA BPDE-DNA
708 BPDE Adducts and Metabolic Polymorphisms
F o EH3mt/mt+EH4wt/wt [6]
U remaining combinations (38]
(23)
�E(17)
IFig. 4. Frequency of detectable adducts in relation to mEH gene polymor-
phisms. EH3 mi/mt and EH4 wi/wi, homozygous mutated on exon 3 and homozy-
gous wild type on exon 4, respectively. Numbers in brackets, total numbers ofsubjects carrying each genotype: numbers in parentheses, numbers of subjects
with detectable adducts. None of the differences were statistically significant.
derline effect in foundry workers. Mooney et a!. (36) reportedthat heavy smokers with CYPIAJ m2 variant alone or in com-bination with GSTMJ null genotype sustained more genetic
damage from cigarette smoking than individuals without these
factors.In our study, subjects with undetectable adducts did not
carry any CYPIA] polymorphism; the presence of at least onevariant in the CYPIAJ gene was significantly associated with
higher frequency of detectable BPDE-SA adducts but not withHb adducts or with DNA adducts. To our knowledge, this is thefirst evidence that the CYP/Al polymorphism influences ad-
ducts other than DNA adducts.CYP/Al polymorphism is often explained as enhanced
inducibility, leading to higher enzymatic activity to activateprecarcinogens. It has been proposed that ml mutation in the 3’
flanking region of the gene might be a marker for alteration onregulatory sites, whereas m2 seems to increase enzymatic ac-
tivity ( I 6, 17). In both cases, the activation of BaP to theultimate carcinogenic BPDE might be enhanced, resulting inhigher levels of SA adducts. This preferential site of adductioncould be easily explained by the fact that adduct formation maybe more efficient with SA because the protein is synthesized inthe liver, in which most xenobiotic metabolism takes place. ButCYPIAI is considered to be primarily an extrahepatic enzyme,so its apparently enhanced activity would not sustain the in-creased formation of BPDE adducts to SA. This apparent dis-crepancy may be due to the influence of CYPIA] polymor-
phisms on the function of CYPIA2, a cytochrome P450 enzymeresponsible for BaP activation in the liver. It has been recently
reported that on exposure to cigarette smoke, individuals withheterozygous variants of CYP/Al gene had significantly in-
creased CYPIA2 activity (43).In our study, the small number of people with the rare m2
allele precluded any analysis stratified by exon 7 genotype,reported to be the “high-risk” polymorphism for lung cancer(17). There was only a suggestion that the m2 variant influ-
enced BPDE-DNA adduct frequency.We focused our attention on a further enzyme involved in
the BaP metabolism: mEH, the polymorphism of which has notbeen evaluated in relation to PAH exposure.
The mutation on exon 3 of the mEH gene (EH3) that
changes Tyr- 1 1 3 to His- 1 13 reduced the enzyme activity, yield-ing a slow allele, whereas the mutation on exon 4 (EH4)
changing His-l39 to Arg-l39 and increased the activity, yield-
ing a fast allele (20).Considering each variant separately, no remarkable effects
on adduct levels or frequency were noted. If the patients areclassified by both polymorphisms, those with two mutated
alleles on exon 3 and no mutation on exon 4 had a lowerfrequency of BPDE-SA adducts and a marginally significant
absence of DNA adducts.The mechanism underlying this finding can be explained
on the basis of mEH enzymatic activity as a function of poly-morphic 113 and 139 amino acid residues.
Patients with two slow alleles (EH3 homozygous mutated)
and no fast allele (EH4 homozygous wild type) are a very slowphenotype for which decreased enzyme activity can be inferred.In the case of BPDE adduct formation, this mEH genotype
might constitute a protective genetic make-up.However, the role of mEH polymorphisms in relation to
cigarette smoke carcinogens has to be evaluated carefully be-cause the mEH slow phenotype has been correlated with in-
creased susceptibility to emphysema, suggesting that the puta-tive decrease in enzyme activity is responsible of the increasedepoxide intermediates involved in the progressive tissue abnor-
malities seen in emphysema (34).The correlation between mEH polymorphism and enzyme
activity needs to be clarified, and a recent study was unable toassign hepatic mEH protein/enzymatic activity levels solely
based on the two polymorphic amino acid loci, suggesting thatadditional factors regulate mEH expression (44).
In conclusion, our findings address the importance ofcomparative biomarker analysis to identify the exposure marker
that most accurately indicates the true dose absorbed. This
explorative investigation shows that BPDE-SA adducts areapparently more easily influenced by genetically determineddifferences in metabolizing BaP than are Hb and lymphocyte
DNA adducts.Although our patients were a homogeneous population
with respect to tobacco BaP exposure, at least in terms of
cigarettes/day and pack-years, the effect of genotypes could notcompletely explain the high variability in adduct levels ob-
served, suggesting others factors, such as type of tobacco or
smoking style, might affect the dose of BaP received.This study brought to light some suggestions of a relation
between the genotypes considered and BPDE adduct formation,
but the small sample size prevented any conclusive inference.
Acknowledgments
We thank Dr. Regina Santella (Columbia University, New York, NY) for the kind
gift of 8E I I monoclonal antibodies and the clinical staff of the Division of
Thoracic Surgery, European Institute of Oncology, Milan, Italy, for their coop-
eration. The editorial assistance of J. Baggots and the staff of the G. A. Pfeiffer
Memorial Library is gratefully acknowledged.
References
I . WHO. Polynuclear aromatic compounds. Part 1 : chemicals, environmental and
experimental data. In: Evaluation of Carcinogenic Risk of Chemicals to Humans,
Vol. 32, IARC Monographs. Lyon, France: IARC, 1983.
2. Perera, F. P., Dickey. C., Santella, R., O’Neill, J. P. 0., Albertini, R. J.,
Ottman, R., Tsai, W-Y., Mooney. L. A., Savela, K., and Hemminki, K. Carcin-
ogen-DNA adducts and gene mutation in foundry workers with low-level expo-
sure to polycyclic aromatic hydrocarbons. Carcinogenesis (Land.), 15: 2905-
2910, 1994.
3. Motykiewicz, G.. Malusecka, E., Grzybowska, E., Chorazy, M., Zhang. Y-J.,
Perera, F. P., and Santella, R. Immunohistochemical quantification of polycyclic
aromatic hydrocarbon-DNA adducts in human lymphocytes. Cancer Res., 55:
1417-1422, 1995.
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

Cancer Epidemiology, Biomarkers & Prevention 709
4. Tas, S., Buchet, J. P., and Lauwerys, R. Determinants of benzo(a)pyrene diol
epoxide adducts to albumin in workers exposed to polycyclic aromatic hydro-
carbons. Int. Arch. Occup. Environ. Health, 66: 343-348, 1994.
5. Tang, D., Santella, R. M., Blackwood, A. M., Young, T-L., Mayer, J., Jaretzki,
A., Grantham, S., Tsai, W-Y., and Perera, F. P. A molecular epidemiology
case-control study of lung cancer. Cancer Epidemiol. Biomark. Prey., 4: 341-346,
1995.
6. Denissenko, M. F., Pao, A., Tang, M-S., and Pfeifer, G. P. Preferential
formation of benzo(a)pyrene adducts at lung cancer mutational hotspots in p53.
Science (Washington DC), 274: 430-432, 1996.
7. Gelboin, H. V. Benzo[a]pyrene metabolism, activation and carcinogenesis:
role and regulation of mixed-function oxidases and related enzymes. Physiol.
Rev., 60: 1107-1166, 1980.
8. Ketterer, B., Harris, J. M., Talaska, G., Meyer, D. J., Pemble, S. E., Taylor,J. B., Lang, N. P., and Kadlubar, F. F. The human glutathione S-transferase
supergene family. its polymorphism, and its effects on susceptibility to lung
cancer. Environ. Health Perspect., 98: 87-94, 1992.
9. Bell, D. A., Thompson, C. L., Taylor, J., Clark, G., Miller, C. R., Perera, F. P.,
Hsieh, L., and Lucier, G. W. Genetic monitoring of human polymorphic cancer
susceptibility genes by polymerase chain reaction: application to glutathione
transferase. Environ. Health Perspect., 98: 1 13-1 17, 1992.
10. Seidegard, J., Pero, R. W., Markowitz, M. M., Roush, G., Miller, D. G., andBattie, E. J. Isoenzyme(s) of glutathione transferase (class p�) as a marker for the
susceptibility to lung cancer: a follow-up study. Carcinogenesis (Lond.). II:33-36. 1990.
11. McWilliams, J. E., Sanderson, B. J. S., Harris, E. L., Richert-Boe, E., and
Henner, W. D. Glutathione S-transferase Ml (GSTMI) deficiency and lungcancer risk. Cancer Epidemiol. Biomark. Prey., 4: 589-594, 1995.
12. Nakachi, K., lami, K., Hayashi, S., Watanabe, J., and Kawajiri, K. Genetic
susceptibility to squamous cell carcinoma of the lung in relation to cigarette
smoking dose. Cancer Res., 51: 5177-5180, 1991.
13. Tefre, T., Ryber, D., Haugen, A., Nebert, D. W., Skaug, V., Brogger. A., and
Borresen, A-L. Human CYPIAI (cytochrome P1-450) gene: lack of association
between the MspI restriction fragment length polymorphism and incidence of
lung cancer in a Norwegian population. Pharmacogenetics. 1: 20-25, 1991.
14. Hirvonen, A., Husgafvel-Pursiainen. K.. Karjalainen, A., Anttila, S., andVainui, H. Point-mutational MspI and Ile-VaI polymorphisms closely linked in
the CYPIAI gene: lack of association with susceptibility to lung cancer in a
Finnish study population. Cancer Epidemiol. Biomark. Prey., 1: 485-489. 1992.
15. Xu, X., Kelsey, K. T., Wiencke, J. K., Wain, J. C., and Christiani, D. C.
Cytochrome P450 CYP1AI MspI polymorphism and lung cancer susceptibility.
Cancer Epidemiol. Biomark. Prey., 5: 687-692, 1996.
16. Kawajiri, K., Nakachi, K., Imai, K., Watanabe, J., and Hayashi, S. The
CYPJAI gene and cancer susceptibility. Crit. Rev. Oncol. Hematol., 14: 77-87,
I 993.
17. Drakoulis, N., Cascorbi, I., Brockmtiller, J., Gross, C. R., and Roots, I.
Polymorphisms in the human CYPJAI gene as susceptibility factors for lung
cancer: exon-7 mutation(4889 A to G), and a T to C mutation in the 3-flanking
region. Clin. Invest., 72: 240-248, 1994.
18. Cascorbi, I., Brockmtiller, J., and Roots, I. A C4887A polymorphism in exon
7 of human CYP1A1: population frequency, mutation linkages and impact on
lung cancer susceptibility. Cancer Res., 56: 4956-4969, 1996.
19. Shields, P. G., Caporaso, N. E., Falk, R. T., Sugimura, H., Trivers, G. E.,
Trump. B. F., Hoover, R. N., Weston, A., and Harris, C. C. Lung cancer, race and
a CYP/Al genetic polymorphism. Cancer Epidemiol. Biomark. Prey., 2: 481-
485, 1993.
20. Hassett, C., Aicher, L., Sidhu, J. S., and Omiecinski, C. J. Human microsomalepoxide hydrolase: genetic polymorphism and functional expression in vitro of
amino acid variants. Hum. Mol. Genet., 3: 421-428, 1994.
21. McGlynn, K. A., Rosvold, E. A., Lustbader, E. D., Hu, Y., Clapper. M. L..
Zhou, T., Wild, C. P., Xis, X-L., Baffoe-Bonnie, A., Ofori-Adjei. D., Chen, G-C.,London, W. T., Shen, F-M., and Buetwo, K. H. Susceptibility to hepatocellular
carcinoma is associated with genetic variation in the enzymatic detoxification ofaflatoxin Bl. Proc. NatI. Acad. Sci. USA. 92: 2384-2387, 1995.
22. Brockm#{246}ller, J., Cascorbi, I., Kerb, R., and Roots I. Combined analysis of
inherited polymorphisms in arylamine N-acetyltransferase 2, glutathione S-trans-
ferase Ml and TI, microsomal epoxide hydrolase and cytochrome P4450 en-zymes as modulators of bladder cancer risk. Cancer Res., 56: 3915-3925, 1996.
23. Lancaster, J. L., Brownlee, H. A., Bell, D. A., Futreal, A., Marks, J. R.,
Berchuck, A., Wiseman, R. W., and Taylor. J. A. Microsomal epoxidehydrolase
polymorphism as a risk factor for ovarian cancer. Mol. Carcinog.. 17: 160-162,
I 996.
24. Shields, P. G., Bowman, E. D., Harrington, A. M., Doan, V. T., and Weston,
A. Polycyclic aromatic hydrocarbon-DNA adducts in human lung and cancer
susceptibility genes. Cancer Res., 53: 3486-3492, 1993.
25. Ryberg, D., Hewer, A., Phillips, D. H., and Haugen, A. Different suscepti-
bility to smoking-induced DNA damage among male and female lung cancer
patients. Cancer Res., 54: 5801-5803, 1994.
26. Ichiba, M., Hagmar, L., Rannug. A., Hogstedt, B., Alexandrie, A-K..
Carstensen, U., and Hemminki, K. Aromatic DNA adducts, micronuclei andgenetic polymorphism for CYPIAI and GST in chimney sweepers. Carcinogen-
esis (Land.), 15: 1347-1352, 1994.
27. Grinberg-Funes, R. A., Singh, V. N., Perera, F. P., Bell, D. A., Young. T. L.,
Dickey. C., Wang. L. W., and Santella, R. M. Polycyclic aromatic hydrocarbon-
DNA adducts in smokers and their relationship to micronutrient levels and the
glutathione-S-transferase MI genotype. Carcinogenesis (Lond.). II: 2449-2454,
1994.
28. Rothman, N., Shields, P. G., Poirier, M. C., l-Iarrington, A. M., Patrick Ford,
D.. and Strickland, P. T. The impact of glutathione S-transferase M I and cyto-
chrome P450 lAl genotypes on white-blood-cell polycyclic aromatic hydrocar-
hon-DNA adduct levels in humans. Mol. Carcinog.. /4: 63-68. 1995.
29. Pastorelli, R., Restano, J., Guanci, M., Maramonte, M., Magagnotti. C.,
Allevi, R.. Lauri, D., Fanelli, R., and Airoldi, L. Hemoglobin adducts of benzo-
(a)pyrene diolepoxide in newspaper vendors: association with traffic exhaust.
Carcinogenesis (Land.), 17: 2389-2394, 1996.
30. Wu, Q., Chen, M., Buchwald, M., and Phillips, R. A. A simple. rapid method
for isolation of high quality genomic DNA from animal tissue. Nucleic Acid Res..
23: 5087-5088. 1995.
31 . Englard. S.. and Seifter. S. Precipitation techniques. In: M. P. Deutscher
(ed), Methods in Enzymology, Vol. 182, Guide to Protein Purification, pp.
285-300. San Diego: Academic Press. Inc.. 1990.
32. Santella, R. M., Lin, C. D., Clevelend, W. L., and Weinstein, I. B. Mono-
clonal antibodies to DNA modified by a benzo(a)pyrene diol epoxide. Carcino-
genesis (Lond.), 5: 373-377, 1984.
33. Bell, D. A., Taylor. J. A.. Paulson, D. F., Robertson, C. N., Moheler, J. L.,
and Lucier, G. W. Genetic risk and carcinogen exposure: a common inherited
defect of the carcinogen-metabolism gene glutathione S-transferase M I (GSTMI)
that increases susceptibility to bladder cancer. J. NatI. Cancer Inst. (Bethesda). 85:
159-164, 1993.
34. Smith, C. A. D., and Harrison, D. J. Association between polymorphism in
gene for microsomal epoxide hydrolase and susceptibility to emphysema. Lancet.
350: 630-633, 1997.
35. SAS Institute Inc. SAS/STAT User’s Guide, Version 6. Ed. 4, Vol. 2, p. 846.
Cary, NC: SAS Institute Inc., 1989.
36. Mooney, L. A., Bell, D. A., Santella, R. M., Van Bennekum, A. M., Ottman.R., Paik, M., Blaner, W., Lucier, G. W., Covey, L., Young. T. L., Cooper. T. B..Glassman, A. H., and Perera, F. P. Contribution of genetic and nutritional factors
to DNA damage in heavy smokers. Carcinogenesis (Land.). 18: 503-509. 1997.
37. Autrup. H.. Vestergaard. A. B., and Okkels, H. Transplacental transfer of
environmental genotoxins: polycyclic aromatic hydrocarbon-albumin in non-
smoking women, and the effect of matemal GSTMI genotype. Carcinogenesis
(Lond.), 16: 1305-1309, 1995.
38. Crawford, F. G., Mayer. J., Santella, R. M., Cooper, T. B.. Ottman, R., Tsai.W-Y., Simon-Cereijido, G.. Wang. M., Tang, D., and Perera, F. P. Biomarkers of
environmental tobacco smoke in preschool children and their mothers. J. NatI.
Cancer Inst. (Bethesda), 86: 1398-1402, 1994.
39. Melikian, A. A., Sun, P., Pierpont, C., Coleman, S., and Hecht, S. S.
Gas-chromatographic-mass spectrometric determination of benzo(a)pyrene and
chrysene diol epoxide globin adducts in humans. Cancer Epidemiol. Biomark.
Prey., 6: 833-839, 1997.
40. Mooney, L. A., Santella, R. M., Covey, L., Jeffrey. A. M., Bigbee, W.,Randall, M. C., Cooper. T. B., Ottman, R., Tsai, W. T., Wazneh, L., Glassman,
A. H., Young, T-L., and Perera, F. P. Decline of DNA damage and other
biomarkers in peripheral blood following smoking cessation. Cancer Epidemiol.
Biomark. Prey., 4: 627-634, 1995.
41. Skipper, P. L., and Tannenbaum, S. R. Protein adducts in the molecular
dosimetry of chemical carcinogens. Carcinogenesis (Land.). II: 507-518. 1990.
42. Hemminki, K., Dickey, C., Karlsson, S., Bell, D., Hsu. Y., Tsai, W-Y.,
Mooney, L. V., Savela, K., and Perera, F. P. Aromatic DNA adducts in foundry
workers in relation to exposure. life style and CYPI A I and glutathione transfer-
ase Ml genotype. Carcinogenesis (Lond.), /8: 345-350. 1997.
43. MacLeod, S., Sinha, R., Kadlubar. F. F.. and Lang. N. P. Polymorphisms of
CYPIAI and GSTMI influence the in vito function of CYPIA2. Mutat. Res.,
376: 135-142, 1997.
44. Hassett, C.. Lin, J., Carty, C. L., Laurenzana, E. M., and Omiecinski, C. J.Human hepatic microsomal epoxide hydrolase: comparative analysis of polymor-
phic expression. Arch. Biochem. Biophys.. 337: 275-283. 997.
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from

1998;7:703-709. Cancer Epidemiol Biomarkers Prev R Pastorelli, M Guanci, A Cerri, et al. benzo(a)pyrene-diolepoxide.on DNA, and blood protein adducts ofM1, microsomal epoxide hydrolase, cytochrome P450 enzymes Impact of inherited polymorphisms in glutathione S-transferase
Updated version
http://cebp.aacrjournals.org/content/7/8/703
Access the most recent version of this article at:
E-mail alerts related to this article or journal.Sign up to receive free email-alerts
Subscriptions
Reprints and
To order reprints of this article or to subscribe to the journal, contact the AACR Publications
Permissions
Rightslink site. Click on "Request Permissions" which will take you to the Copyright Clearance Center's (CCC)
.http://cebp.aacrjournals.org/content/7/8/703To request permission to re-use all or part of this article, use this link
Association for Cancer Research. by guest on October 24, 2020. Copyright 1998 Americanhttps://bloodcancerdiscov.aacrjournals.orgDownloaded from