Testo Tumori Esofago Xst
Transcript of Testo Tumori Esofago Xst

OESOPHAGEAL TUMOURS

Avvertenza per gli studenti del corso di Anatomia Patologica del corso Integrato Malattie dell’apparato Gastroenterico e
Infettive.
Questi appunti sono solo una traccia di ciò che ho svolto a lezione. Non possono e non vogliono sostituire la trattazione degli stessi argomenti sui libri di testo e non esimono dallo
studio degli altri argomenti del programma.Infine, devono essere utilizzati solo per uso personale del
singolo studente.
Buon studio
Achille PICH

Principi della classificazione WHOdei Tumori
PRIMITIVI1) Tumori epiteliali benigni e lesioni pseudotumorali2) Tumori non-epiteliali benigni3) Tumori epiteliali maligni
4) Tumori non-epiteliali maligni
SECONDARIEpitelialiNon-epiteliali

Histological classification WHO
Benign– Squamous cell papilloma– Viral wart– Adenoma
Epithelial tumours

– Squamous cell carcinoma•Verrucous (squamous) carcinoma•Spindle cell (squamous) carcinoma
Histological classification WHO
Epithelial tumours
Malignant

Epithelial tumours
– Adenocarcinoma•Adenosquamous carcinoma•Mucoepidermoid carcinoma•Adenoid cystic carcinoma
– Small cell carcinoma– Undifferentiated carcinoma– Others
Malignant
Histological classification WHO

Histological classification WHO
– Leiomyoma– Lipoma– Vascular tumours– Neurogenic tumours– Granular cell tumours– Others: GIST
Non-epithelial tumoursBenign

Histological classification WHO
– Leiomyosarcoma– Kaposi sarcoma– Others
Non-epithelial tumours
Malignant

Histological classification WHO
Tumour-like lesions– Fibrovascular (fibrous) polyp– Cysts – Inflammatory polyp– Glycogenic acanthosis– Diffuse leiomyomatosis– Gastric heterotopia
Miscellaneous tumours– Malignant melanoma– Others– CarcinosarcomaSecondary tumours

Histological classification WHO
Benign– Squamous cell papilloma– Viral wart– Adenoma
Epithelial tumours

Histological classification WHO
– Leiomyoma– Lipoma– Vascular tumours– Neurogenic tumours– Granular cell tumours– Others: GIST
Non-epithelial tumoursBenign

Leiomyomas are the most common benign tumors of the esophagus. In careful autopsy cases, the frequency of this lesion has been found to be almost 8%. Half of the surgically excised cases are asymptomatic; dysphagia and vague thoracic pain are the main complaints in the others. The majority arise from the inner circular muscle and are more common in the distal third. Ulceration of the overlying mucosa is a rare event, in contrast to its common occurrence in gastric leiomyomas.Local resection or enucleation is usually successful.

EPITHELIAL ABNORMALITIES(Precancerous)
Dysplasia and carcinoma in situin squamous epithelium

Leukoplakia

Dysplasia
Grade 1Grade 2Grade 3

Carcinoma “in situ”

– Squamous cell carcinoma•Verrucous (squamous) carcinoma•Spindle cell (squamous) carcinoma
Histological classification WHO
Epithelial tumoursMalignant

It is relatively common in China and other Oriental countries (130/100.000) and is the most common tumor of the alimentary tract in the African Bantus (70/100.000). In the United States it is less common (5.5% of G.I. tumors).
Smoking (3-5x) and alcohol (50g/die: 4x; 100g/die: 20x) are two important and well-known risk factors.
Squamous cell carcinoma of the esophagus occurs more frequently in men (5:1) over 50 years of age.

Association may occur with squamous cell carcinoma in other sites, particularly the oropharynx and larynx (12%); sometimes, with gastric adenocarcinoma.
Association is described with lye strictures, achalasia, Plummer Vinson syndrome, diverticula, celiac sprue, tylosis (an auto-somal dominant disorder characterized by hyperkeratosis of palms and soles), and history of previous irradiation.
Increased incidence of esophagitis and a history of previous gastrectomy is described in patients with esophageal squamous cell carcinoma.

It has been suggested that HPV might play an etiologic role in esophageal carcinogenesis either by producing carcinogens or promotors or by acting directly on the host cells. In several studies, DNA sequences of HPV have been found in a percentage (up to 60%) of cases of esophageal squamous cell carcinoma.

HISTOLOGICAL GRADING
G1G2G3
Well differentiatedMedium differentiatedPoorly differentiated

TNM Clinical Classification
Tis Carcinoma in situ/high grade dysplasiaT1 Lamina propria, muscolaris mucosae or
submucosaT1a Lamina propria or muscolaris mucosaeT1b Submucosa
T2 Muscularis propriaT3 AdventitiaT4 Adjacent structures
T4a Pleura, pericardium or diaphragmT4b Aorta, vertebral body, or trachea
TX Primary tumour cannot be assessedT0 No evidence of primary tumour

N0 No metastasis in regional nodesN1 Metastasis in 1-2 regional nodes
M0 No distant metastasisM1 Distant metastasis
NX Regional nodes cannot be assessed
N2 Metastasis in 3-6 regional nodesN3 Metastasis in 7 or more regional nodes
TNM Clinical Classification

STAGE GROUPING (1)
Stage 0
Stage IA
Stage IB
Stage IIB
Tis
T1
T2
T1, T2
N0
N0
N0
N1
M0
M0
M0
M0T3 N0 M0Stage IIA

STAGE GROUPING (2)
Stage IIIC
Stage IV Any T Any N M1
T4a M0N1,N2
Stage IIIB
T3
T3
N1
N2
M0
M0
T4a N0 M0
T1,T2 M0N2
Stage IIIA
T4b M0Any NAny T M0N3

Prognostic Factors

Prognosis is very poor: the median survival after diagnosis is less than 1 year.
1. Sex. Better survival in females.
2. Stage: is of paramount importance.
3. Microscopic grade: not substantial.
4. Other microscopic findings: vascular or lymphatic invasion and marked tumor necrosis worse prognosis; peritumoral fibrosis and lymphocytic reaction better prognosis.

5. Surgical margins.
6. DNA ploidy and proliferation indices: aneuploidy and high AgNOR counts poor prognosis.
7. Epidermal growth factor receptor (EGFR). Over-expression poor prognosis.
8. p53. Overexpression worse survival.

– Squamous cell carcinoma•Verrucous (squamous) carcinoma•Spindle cell (squamous) carcinoma
Histological classification WHO
Epithelial tumours
Malignant

Verrucous carcinoma, morphologically identical to its more common counterpart in the oral cavity, has been described in the esophagus.
It is grossly polypoid and well differentiated throughout microscopically. Despite these features and its inability to metastasize, the mortality associated with this tumor is high.

– Squamous cell carcinoma•Verrucous (squamous) carcinoma•Spindle cell (squamous) carcinoma
Histological classification WHO
Epithelial tumours
Malignant

Squamous cell carcinoma with spindle-cell stroma (pseudosarcoma; carcinosarcoma; spindle cell carcinoma; polypoid carcinoma) usually presents as a large polypoid neoplasm.
Metastases or recurrences supervene in about 20% of the patients undergoing surgery, and the overall survival rate is in the neighborhood of 50%

The bulk of the tumor has a pleomorphic sarcoma-like
appearance. Most evidence suggests that this component
is also of epithelial derivation. Ultrastructurally, some of
these sarcoma-like cells in some of the tumors retain
epithelial markers, such as desmosomes and tonofibrils.
Immunohistochemically, keratin can be consistently
demonstrated in the epithelial-appearing component and,
in a high proportion of cases, also in some of the
sarcoma-like cells. The latter also exhibit strong reactivity
for vimentin and occasionally for actin and desmin.

Epithelial tumours
– Adenocarcinoma•Adenosquamous carcinoma•Mucoepidermoid carcinoma•Adenoid cystic carcinoma
– Small cell carcinoma– Undifferentiated carcinoma– Others
Malignant
Histological classification WHO

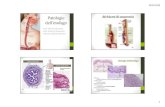
Esofagite da riflussoEsofagite da riflusso
The esophageal mucosa reacts to reflux by hyperplasia of the basal layer, The esophageal mucosa reacts to reflux by hyperplasia of the basal layer, elongation of stromal vascular papillae, and infiltration with inflammatory elongation of stromal vascular papillae, and infiltration with inflammatory cells, often including eosinophils. Complications include ulceration, cells, often including eosinophils. Complications include ulceration, stricture and replacement of the squamous epithelium by columnar stricture and replacement of the squamous epithelium by columnar epithelium, a metaplastic process that results in: epithelium, a metaplastic process that results in:
Barrett's esophagus Barrett's esophagus
This occurs in about 10% of patients with reflux esophagitis and is This occurs in about 10% of patients with reflux esophagitis and is significant because 5-10% of such patients develop adenocarcinoma. significant because 5-10% of such patients develop adenocarcinoma.
Barrett's mucosa may be of Barrett's mucosa may be of cardiac, fundal, or intestinal typecardiac, fundal, or intestinal type. Usually a . Usually a mixture of all three types is present. Adenocarcinoma appears to arise mixture of all three types is present. Adenocarcinoma appears to arise predominantly in the intestinal type mucosa with dysplasia as a precursor predominantly in the intestinal type mucosa with dysplasia as a precursor lesion. Complications other than carcinoma include ulcer and stricture. lesion. Complications other than carcinoma include ulcer and stricture.

Adenocarcinoma of the esophagus can arise from Barrett's metaplastic mucosa, from a focus of heterotopic gastric mucosa, or, theoretically, from esophageal glands.
Adenocarcinomas make up about 10% of esophageal cancers, but their relative frequency seems to be on the rise (→40%).
A very small proportion of primary esophageal adenocarcinomas have “signet ring cell” features.

Epithelial tumours
– Adenocarcinoma•Adenosquamous carcinoma•Mucoepidermoid carcinoma•Adenoid cystic carcinoma
– Small cell carcinoma– Undifferentiated carcinoma– Others
Malignant
Histological classification WHO

Small cell carcinoma (neuroendocrine carcinoma; anaplastic small cell carcinoma) is a highly malignant esophageal tumor composed of anaplastic small cells. Argyrophilic granules can be demonstrated.
Some cases have been associated with ACTH and serotonin production.
The prognosis is very poor; most patients die quickly with generalized metastases.

Histological classification WHO
Tumour-like lesions– Fibrovascular (fibrous) polyp– Cysts – Inflammatory polyp– Glycogenic acanthosis– Diffuse leiomyomatosis– Gastric heterotopia
Miscellaneous tumours– Malignant melanoma
– Others– Carcinosarcoma
Secondary tumours

Malignant melanoma can be located at any level in the esophagus, but it has a predilection for the lower third. Grossly, the tumor is usually large and has a prominent polypoid appearance. Microscopically, epithelioid, spindle-cell, and pleomorphic areas may be seen singly or in combination. The amount of melanin produced is highly variable. Immunohistochemically, S-100 protein and HMB 45 positivity are the rule. The prognosis is exceedingly poor.

Histological classification WHO
Tumour-like lesions– Fibrovascular (fibrous) polyp– Cysts – Inflammatory polyp– Glycogenic acanthosis– Diffuse leiomyomatosis– Gastric heterotopia
Miscellaneous tumours– Malignant melanoma– Others– CarcinosarcomaSecondary tumours

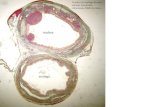
Esophageal cysts are classified into: - inclusion cysts (lined by squamous or columnar epithelium, sometimes ciliated), - retention cysts or mucoceles (arising from cystic dilatation of submucosal glands), and - developmental cysts (of esophageal, bronchial, or gastric origin).
Cases of squamous cell carcinoma or adenocarcinoma arising in such cysts have been reported








![acalasia1.ppt [modalità compatibilità] · Ipermotilità ipercontrattileIpermotilità ipercontrattile Esofago a sciaccianoci 48%Esofago a sciaccianoci 48% Normale peristalsiNormale](https://static.fdocumenti.com/doc/165x107/5c69a9c609d3f2310b8b6cca/modalita-compatibilita-ipermotilita-ipercontrattileipermotilita-ipercontrattile.jpg)