Test genomici e Medicina Personalizzata · Test genomici e Medicina Personalizzata Valentina...
Transcript of Test genomici e Medicina Personalizzata · Test genomici e Medicina Personalizzata Valentina...
Test genomici e Medicina PersonalizzataValentina GuarneriIstituto Oncologico Veneto IRCCS
Dipartimento di Scienze Chirurgiche, Oncologiche e Gastroenterologiche –
DiSCOG, Università di Padova
• Understand tumor biology• Dissect tumor heterogeneity
• Determine pathways driving cancer growth and
treatment resistance
• Identify potential targets in tumor cells or the
microenvironment
• Assess the risk of recurrence
• Assess treatment benefit
Goals of personalized medicine
Prognostic factors
Risk Assessment
Prognostic factorsAge, T, N, histology, grade, LVI, Ki-67, HR, HER2
Predictive factorsHR, HER2
Proportional
benefit
Absolute benefit
Adjuvant Rx of EBC - Decision-making Algorithm
Short- and Long-
term toxicities
Patient
Characteristics
and preference
Adjuvant medical treatments
Reis-Filho J, Lancet 2011
Class discovery
Mammaprint
Endopredict
GGI
BCI
OncotypeDX
Top-Down
approach
Bottom-up
approach
Candidate gene
approach
PAM50 - ROR
� Same entity of proportional risk reductions
across age, nodal status, T size and ER
status groups.
� The same proportional risk reduction
translates into different absolute
reductions according to absolute risk
without chemotherapy.
EBCTCG, Lancet 2012
Anthracycline-based CT vs no CT
Can we define a very-low risk group that,
whatever the relative benfit is, could be
spared adjuvant chemotherapy?
Clinical validity Predict baseline prognosis
Clinical utility Who can be spared a more aggressive treatment?
An ABSOLUTE issue: Prognosis is so good that the relative
benefit, if any, would translate into an unrelevant absolute
gain
Target pts (VERY) LOW RISK
(don’t mind what the relative benfit would be)
Paik NEJM 2006 Vijver NEJM 2002Dowsett JCO 2013 Filipits CCR 2011
MammaPrintOncotypeDX PAM50 ROR EndoPredict
(include tumor size+nodal status)
Genomic profiling predicting baseline prognosis for HR+/HER2- patients
Van’t Veer L. et al, Nature 2002
Relapse
No relapse
70 genes identified after supervised
analysis of 250000 genes
Independent cohort:295
consecutive patients with stage I or
II breast cancer, < 53 years old; 151
had lymph-node-negative disease,
and 144 had lymph-node-positive
disease
Van de Vijver MJ, et al, NEJM 347:1999-2009, 2002
Mammaprint: 70-genes prognostic signature
MINDACT Trial design (n=6000)
Node negative & 1-3 positive nodes
Primary objective:
• Confirm that CLINPATH HIGH / MammaPrint LOW
patients can safely avoid chemotherapy
Null hypothesis: 5-yrs DMFS for CLINPATH HIGH /
MammaPrint LOW pts randomized to NO CHEMO is 92%;
reject the null hypothesis if DMFS 95%.
16 Cancer and 5 Reference Genes From 3 Studies
PROLIFERATION
Ki-67
STK15
Survivin
Cyclin B1
MYBL2
ESTROGEN
ER
PR
Bcl2
SCUBE2
INVASION
Stromolysin 3
Cathepsin L2
HER2
GRB7
HER2
BAG1GSTM1
REFERENCE
Beta-actin
GAPDH
RPLPO
GUS
TFRC
CD68
Paik S, NEJM 351(27):2817, 2004
RS = + 0.47 x HER2 group core
- 0.34 x HR group score
+ 1.04 x proliferation group score
+ 0.10 x invasion group score
+ 0.05 x CD 68
- 0.08 x GSTM1
- 0.07 x BAG1
RS < 18 RS 18-30 RS > 31
The Oncotype DX® 21 Gene Recurrence Score (RS) Assay: continuous predictor
Distant recurrence over time
10-Year rate of recurrence = 6.8%*95% CI: 4.0%, 9.6%
0 2 4 6 8 10 12 14 16
Years
Paik S, et al. N Engl J Med. 2004;351:2817-2826.
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Pro
po
rtio
n w
ith
ou
t d
ista
nt
rec
urr
en
ce
RS < 18, n = 338
RS 18-30, n = 149
RS ≥ 31, n = 181
All Patients, n = 668
P < 0.001
10-Year rate of recurrence = 14.3%95% CI: 8.3%, 20.3%
10-Year rate of recurrence = 30.5%*95% CI: 23.6%, 37.4%
*10-Year distant recurrence comparison between low- and high-risk groups: P < 0.001
RS, Recurrence Score® result
Clinical validation study including 668 pts
from the NSABP B-14 trial (stage I-II, N-,
ER+ treated with 5 yrs of TAM)
Oncotype DX® Clinical Validation:
Prognosis in N- ER+ TAM-treated (NSABP B14)
Oncotype DX® assayOncotype DX® assay
Primary study group
RS 11–25
Primary study group
RS 11–25RS >25RS >25RS <11RS <11
RandomizeRandomizeARM D: CT plus
endocrine therapy
ARM D: CT plus
endocrine therapy
ARM A: endocrine
therapy alone
ARM A: endocrine
therapy alone
ARM C: CT plus
endocrine therapy
ARM C: CT plus
endocrine therapy
ARM B: endocrine
therapy alone
ARM B: endocrine
therapy alone
N=1626 (15.9%)
N=6897 (67.3%)
N=1730 (16.9%)
Enrolled 10,071 pts
(2006-2010) 900 sites, 6 countries
Sparano JA et al. N Engl J Med 2015
Designed to determine whether HT is not inferior to CT+HT in women whose tumors fall in the Primary
Study Group category (RS 11-25). The primary study endpoint is disease-free survival. Other co-primary
endpoints include distant recurrence-free interval, recurrence-free interval, and overall survival.
Trial Assigning IndividuaLized Options
for Treatment (Rx), or TAILORx
RS 0-10 RS 11-25 p
All 1626 (15.9%) 6897 (67.3%)
Age, median (range) 58 (50-64) 55 (48-62) <0.001
Menopausal
post
pre
1143 (70%)
480 (30%)
4396 (64%)
2477 (36%) <0.001
T, median (range) 1.5 (1.2-2.0) 1.5 (1.2-2.0) 0.31
G1
G2
G3
530 (34%)
937 (59%)
111 (7%)
1941 (29%)
3812 (57%)
912 (14%) <0.001
PgR neg
PgR pos
28 (2%)
1562 (98%)
528 (8%)
6224 (92%) <0.001
TailorX: RS low patients’ characteristics
Sparano J, et al. N Engl J Med 2015
5yrs rate 93.8%
(95% CI, 92.4 to 94.9)
5yrs rate 99.3%
(95% CI, 98.7 to 99.6)
5yrs rate 98.7%
(95% CI, 97.9 to 99.2)
5 yrs rate 98.0%
(95% CI, 97.1 to 98.6)
TailorX: prognosis of RS low patients
Sparano J, et al. N Engl J Med 2015
Clinical validity Predict benefit of chemotherapy
Clinical utility Who need (or not need) a more aggressive treatment?
A RELATIVE and BALANCE issue
- Determine the relative benefit and the prognosis,
then balance for absolute gain and toxicity.
Target pts ALL PATIENTS, EXCLUDING VERY LOW
AND VERY HIGH RISKS
Paik S JCO 2006
RS<18
RS 18-30 RS ≥31
RS: prediction of chemotherapy benefit in ER+/N-
NSABP B-20 trial - (ER+, node negative) - Tamoxifen versus CMF/TAM
Benefit of chemo is the same in both
stage-defined risk groups, provided the
RS is high � predictive effect of RS above
underlining risk?
Albain K, Lancet Oncol 2010
RS: prediction of chemotherapy benefit in ER+ N+
Oncotype DX® assayOncotype DX® assay
Primary study group
RS 11–25
Primary study group
RS 11–25RS >25RS >25RS <11RS <11
RandomizeRandomizeARM D: CT plus
endocrine therapy
ARM D: CT plus
endocrine therapy
ARM A: endocrine
therapy alone
ARM A: endocrine
therapy alone
ARM C: CT plus
endocrine therapy
ARM C: CT plus
endocrine therapy
ARM B: endocrine
therapy alone
ARM B: endocrine
therapy alone
N=1626 (15.9%)
N=6897 (67.3%)
N=1730 (16.9%)
Enrolled 10,071 pts
(2006-2010) 900 sites, 6 countries
Sparano JA et al. N Engl J Med 2015
Designed to determine whether HT is not inferior to CT+HT in women whose tumors fall in the Primary
Study Group category (RS 11-25). The primary study endpoint is disease-free survival. Other co-primary
endpoints include distant recurrence-free interval, recurrence-free interval, and overall survival.
Trial Assigning IndividuaLized Options
for Treatment (Rx), or TAILORx
A Phase III, Randomized Clinical Trial of Standard Adjuvant Endocrine Therapy +/-
Chemotherapy in Patients with 1-3 Positive Nodes, HR+/HER2-negative and
HER2-Negative Breast Cancer With Recurrence Score (RS) of 25 or Less.
ClinicalTrials.gov Identifier: NCT01272037
Opened 2011, Estimated Accrual = 4000
Primary Objective:
• To find a significant interaction between Recurrence
Score (as a continuous variable) and treatment
• DFS
• Type 1 error: 5% ; 80% power
Biology vs Stage: is the verdict already clear?
Is there a simpler and cheaper method to
capture the same biologic features as GEP?
GEP vs clinicopathological classical parameters in
predicting baseline prognosis
10
0
9-Y
ea
r ri
sk o
f d
ista
nt
recu
rre
nce
(%
)
Recurrence Score
Node negative
n = 872
1-3 Positive nodes
n = 243
≥ 4 Positive nodes
n = 63
01
02
03
04
05
06
07
08
09
0
0 5 10 15 20 25 30 35 40 45 50
95% CI
Mean
Low Recurrence Score suggests a low risk of recurrence for patients with 1-3 positive nodes.
Dowsett M, et al. J Clin Oncol. 2010;28(11):1829-1834.24
Trans ATAC: rate of distant recurrence increases
with number of positive nodes
for all RS values
Tang G JCO 2011
• Pathologic variables (i.e. grade, tumor size and nodal status) retained
an independent prognostic value which is not captured by the
molecular signature.
Pathologic variables still matter
Ki67: high intralaboratory concordance but low interlaboratory concordance
100 cases, 8 laboratories
Each laboratory: 2 sets of TMA with the same 100 cases
1. Centrally stained, locally scored 2. Locally stained, locally scored
Polley MC, JNCI 2013
Ki67: reproducibility
Breast-DX Italy: Impact of the Oncotype DX® Breast Cancer Assay on
Resources Optimization and Treatment Decisions for Women with
Estrogen Receptor-Positive, Node-Negative and Node-Positive Breast
Carcinoma: a prospective Italian multicenter study.
PROGRAMMA PER LA RICERCA INNOVAZIONE E HTA (PRIHTA) – REGIONE DEL VENETO
Coordinatore: Istituto Oncologico Veneto IRCCS, Padova PI: Prof. PierFranco Conte
- Prospective, multicenter study (ROV)
- To evaluate the impact of Oncotype DX® on thedecision making processes of physicians inrecommending adjuvant therapy and on resourcesoptimization in an Italian setting
OBSERVATIONAL PHASE:
ALL CONSECUTIVE ER+, HER2-, N0-3, T1-3 PATIENTS
Low-Risk at least 4
of the following:
-Data collection
-Physician’s perception of Oncotype DX utility
-Pre-test Physician decision
-Test
-Post-test Physician decision + post-test
perception of utility
-Treatment started
High-Risk at least 4
of the following:CLINICAL PHASE:
SUBGROUP OF PTS FROM THE
OBSERVATIONAL PHASE
Oncotype DX Request for pts not eligible for the Clinical Phase will not be processed by GH.
�G1
�T1a-b
�Ki67 <15%
�N negative
�ER >80%
EXCLUDED
�G3
�T>2
�Ki67 >30%
�N pos
�ER <30%
EXCLUDED
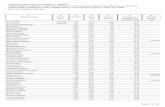
Breast-DX Italy
Centres PI
Oncologia medica 2, Istituto Oncologico Veneto IRCCS - Padova P. Conte
Oncologia Medica, Ospedale di Camposampiero M. Mion
Oncologia Medica, Ospedale dell’Angelo - Mestre P. Morandi
Oncologia Medica, Ospedale di Montecchio Maggiore C. Oliani
Oncologia Medica, Ospedale Borgo Roma - Verona G. Tortora
UOC Oncologia Medica, Ospedale Sacro Cuore don Calabria - Negrar S. Gori
UOC Oncologia Medica, Ospedale di Vicenza L. Merlini
Oncologia Medica, Ospedali di Este e Monselice G. Bonciarelli
Oncologia Medica, Ospedale di Rovigo F. Pasini
Breast-DX Italy: participating centres