Epidemiologia e clinica delle infezioni da virus Zika · Una questione di preferenze… •Aedes...
Transcript of Epidemiologia e clinica delle infezioni da virus Zika · Una questione di preferenze… •Aedes...
Epidemiologia e clinica delle infezioni da virus Zika
Massimo Galli
Clinica delle Malattie Infettive,DIBIC L.Sacco, Università di Mi
Chikungunya è sbarcato in America…. e si è trovato bene !
• Prima del 2013, epidemie di chikungunya erano state descritte solo in Africa, Asia, Europa, e in isole dell’ Oceano Indiano e Pacifico
• Alla fine del 2013 prime trasmissioni in area caraibica
• Da allora osservate epidemie in 45 paesi del continente americano per un totale di più di 1.7 milioni di casi sospetti.
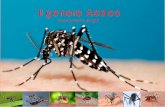
Ae. albopictus
ha una linea bianca su capo e dorso
Ae.aegypti
ha un disegno
a forma di lira sul dorso
Una questione di preferenze…
• Aedes aegypti and Aedes albopictus are known as good dengue vectors in Brazil.
• However, A aegypti plays a major part in dengue transmission in the country due to its vectorial capacity, whereas A albopictus does not because its level of infestation is low and it prefers sylvatic environments.
Ayres CFJ Lancet Infect Dis 2016
Aedes aegypti: una reintroduzione possibile?
• Sulla base di riferimenti storici su epidemie di febbre gialla in Francia e Spagna, si ritiene che Ae.aegypti si sia diffusa in Europa meridionale alla fine del XVII secolo, con possibili reintroduzioni successive in area mediterranea. Aeger JM. Bull Yellow Fever Institute 1902; 3: 1–2
• Nel corso dei secoli XVIII e XIX si sarebbero verificate epidemie di dengue in città portuali del Mediterraneo, tra cui Napoli nel 1889-90.
Schaffner F, Mathis A. Lancet Infect Dis 2014; 14: 1271–80
• Ae. aegypti era presente negli anni ’50 del secolo scorso in tutti i paesi mediterranei e nei paesi costieri del Mar Nero e del Mar Caspio, al di sotto dei 44° e 30’ di latitudine Nord, per poi scomparire dall’inizio degli anni ’60.
• L’ultima, sporadica osservazione in Italia risale al 1972 Callot J, Delecolle J-C. Ann Parasitol Hum Comp 1972; 47: 665
• Ae.aegypti è oggi assente in Europa occidentale, ma ha ricolonizzato nel 2008 le coste del Mar Nero
Yunicheva YU,et al.Med Parazitol Parazit Bol 2008; 3: 40–43
Una lezione da Madeira
• Ae.aegypti è stata reintrodotta almeno dal 2004 l’isola di Madera (Portogallo)
Almeida APG, et al. Euro Surveill 2007; 12: E071115.6
• Nel 2012 sono stati registrati 2144 casi di dengue, 122 dei quali ospedalizzati
Bhatt S, et al. Nature 2013; 496:504.
• Responsabile un virus del sierotipo 1, proveniente dal Sud America.
Alves MJ, et al. Euro Surveill. 2013; 18:pii:20398
• Anche il vettore sarebbe stato recentemente reintrodotto dal Sud America a partire da una ristrettissima popolazione fondante.Seixas G, et al. Mem Inst Oswaldo Cruz, 2013; 108 (S1): 3-10
ZIKV
•ZIKV is a Aedes mosquitoes transmitted flavivirus first isolated from a monkey (a ‘sentinel’ Macacus rhesus) in 1952 in the Zika forest in Uganda.
•Animal reservoir is still unknown
Zika Virus Transmission Cycle.
•In Africa, Zika virus exists in a sylvatic transmission cycle involving nonhuman primates and forest- •dwelling species of aedes mosquitoes . •In Asia, a sylvatic transmission cycle has not yet been identified. Several mosquito species, primarily belonging to the stegomyia and diceromyia subgenera of aedes, including Ae. africanus, Ae. luteocephalus, Ae. furcifer, and Ae. taylori, are likely enzootic vectors in Africa and Asia
Diallo D, et al.PLoS ONE 2014;9: e109442
ZIKV was detected in 31 of the 1,700 mosquito pools (11,247 mosquitoes) tested: Ae. furcifer (5), Ae. luteocephalus (5), Ae. africanus (5), Ae. vittatus (3), Ae. taylori, Ae. dalzieli, Ae. hirsutus and Ae.metallicus (2 each) and Ae. aegypti, Ae. unilinaetus, Ma. uniformis, Cx. perfuscus and An. coustani (1 pool each)
• All the species tested here were susceptible to oral infection of ZIKV but only a low proportion of Ae.vittatus and Ae. luteocephalus had the viral genome in their saliva and thus the potential to transmit the virus.
• Further investigations are needed on the vector competence of other species associated with ZIKV for better understanding of the ecology and epidemiology of this virus in Senegal
Sexual transmission of ZIKV • Sexual transmission to partners of returning male
travelers who acquired Zika virus infection abroad has been reported1-3. In one instance,sexual intercourse occurred only before the onset of symptoms, whereas in other cases sexual intercourse occurred during the development of symptoms and shortly thereafter.
• Replicative viral particles, as well as viral RNA — often in high copy numbers — have been identified in sperm, and viral RNA has been detected up to 62 days after the onset of symptoms4-6.
• 1Foy BD, EID 2011; 17: 880-2.2MMWR 2016; 65: 215-6.3Venturi G, et al. Euro Surveill 2016; 21(8). 4Musso D, et al. EID 2015; 21: 359-61.5Atkinson B,et al. EID 2016 May (Epub ahead of print). 6Mansuy JM, et al. Lancet Infect Dis 2016 March 3 (Epub ahead of print).
Areas in Which Zika Virus Infections in Humans Have Been Noted in the Past
Decade (as of March 2016).
Petersen et al. 30.3.16
ZIKV fever • ZIKV infection in humans symptoms ranges from
asymptomatic to influenza like symptoms
• Common symptoms were macular or papular rash (90% of patients), fever (65%), arthritis or arthralgia (65%), nonpurulent conjunctivitis (55%), myalgia (48%), headache (45%), retro-orbital pain (39%), edema (19%), and vomiting (10%), malaise, anorexia, rash, asthenia, lymphadenopathy, and diarrhoea.
• The rash is generally maculopapular and pruritic, and fever,
• when present, is generally short-term and lowgrade.
• The non-specific clinical presentation can be confused with most other arboviruses particularly DENV and CHIKV infections, even if ZIKV fever is usually milder.
• About 20% of ZIKV-infected people develop these symptoms, while the rest of the infections are asymptomatic
ZIKV infection during pregnancy
• Transmission of ZIKV to the fetus has been documented in all trimesters.
• Zika virus RNA has been detected in fetal tissue from early missed abortions, amniotic fluid, term neonates and the placenta.
• Uncertainties include the incidence of Zika virus infection among pregnant women in areas of Zika virus transmission, the rate of vertical transmission and the rate with which infected fetuses manifest complications such as microcephaly or demise.
Notified cases of microcephaly in Brazil from 2010 to 2015, with 14 states under investigation, as of 28 November 2015
Electron Microscopy of Ultrathin Sections of Fetal Brain and Staining of a Flavivirus-like Particle.
Mlakar et al NEJM Feb 2016
Diagnosis
• In most instances viremia is transient, and diagnosis by RT-PCR has been most successful within 1 week after the onset of clinical illness.
• Viremia is generally low level, which makes viral isolation from clinical samples difficult.
• The precise timing of the onset and the duration of the IgM antibody response to Zika virus that is detectable by MAC-ELISA have not yet been defined,.
ZIKV fetal brain disruption
• Although previous case reports of maternal infection leading to fetal brain disruption sequence do not include information on the timing of maternal infection, some evidence indicates that this damage can occur late during the second trimester or even early in the third trimester.
Mlakar et al NEJM Feb 2016
Neurodevelopmental disorders that cause congenital microcephaly
• Inherited genetic disorders
• Brain injury due to teratogenic drugs, toxins and chemical products, including foetal alcohol syndrome
• Metabolic diseases
• Malnutrition (maternal malnutrition, maternal folate deficiency, placental insufficiency)
• Hypoxic-ischemic lesions
• Infections: transplacental infections of the central nervous system most commonly due to syphilis, toxoplasmosis, rubella, cytomegalovirus and herpes simplex virus (STORCH infections).
• The mean DQ score was 86.3 (95%CI: 81.0–91.5) in infected children compared to 100.2 (95%CI: 98.0–102.5) in uninfected peers (P,0.001).
• Fifty-one percent (n = 17) of infected children had a GND compared to 15% (n = 21) of uninfected children (P,0.001).
• Specific neurocognitive delays in p-CHIKV-infected children were as follows: coordination and language (57%), sociability (36%), movement/posture (27%). After adjustment for maternal social situation, small for gestational age, and head circumference, p-CHIKV infection was found associated with GND (incidence rate ratio: 2.79, 95%CI: 1.45–5.34).
• Of the 12 cases of CHIKV neonatal encephalopathy, five developed a microcephaly (head circumference ,22 standard deviations) and four matched the definition of cerebralpalsy.
Neurologic Complications
• A temporal and geographic relationship has been observed between Guillain–Barré syndrome and Zika virus outbreaks in the Pacific and the Americas.
• In the outbreak in French Polynesia, 38 cases of Guillain–Barré syndrome occurred among an estimated 28,000 persons who sought medical care 1.
• A case–control study in French Polynesia revealed a strong association (odds ratio, >34) between Guillain–Barré syndrome and previous Zika virus infection; the findings from electrophysiological studies were compatible with the acute motor axonal neuropathy subtype of Guillain–Barré syndrome2
• Meningoencephalitis3 and acute myelitis4 also have been reported.
1Cao-Lormeau VM, et al. EID 2014; 20: 1085-6. 2 Cao-Lormeau VM, et al. Lancet 2016 February 29 (Epub ahead of print). 3Carteaux G,et al. NEJM 2016 March 9 (Epub ahead of print). 4Mécharles S, et al. Lancet 2016 March 3 (Epub ahead of print).
Guillain-Barré Syndrome outbreak associated with Zika virusinfection in French Polynesia: a case-control study
• 42 patients were diagnosed with Guillain-Barré syndrome during the study period. 41 (98%) patients with G-BS had anti-Zika virus IgM or IgG, and all (100%) had neutralising antibodies against Zika virus compared with 54 (56%) of 98 in control group 1 (p<0·0001).
• 39 (93%) patients with G-BS had Zika virus IgM and 37 (88%) had experienced a transient illness in a median of 6 days (IQR 4–10) before the onset of neurological symptoms, suggesting recent Zika virus infection. Patients with Guillain-Barré syndrome had electrophysiological findings compatible with acute motor axonal neuropathy (AMAN) type, and had rapid evolution of disease (median duration of the installation and plateau phases was 6 [IQR 4–9] and 4 days [3–10], respectively).
• 12 (29%) patients required respiratory assistance. No patients died.
• Anti-glycolipid antibody activity was found in 13 (31%) patients, and notably against GA1 in eight (19%) patients, by ELISA and 19 (46%) of 41 by glycoarray at admission.
• The typical AMAN-associated anti-ganglioside antibodies were rarely present.
• Past dengue virus history did not differ significantly between patients with Gu-BS and those in the two control groups (95%, 89%, and 83%, respectively).
Cao-Lormeau VM, et al. Lancet 2016 February 29 (Epub ahead of print).
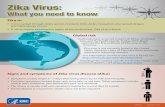
Prevenzione dell’infezione da virus Zika
• La prevenzione e il controllo si basano sulla riduzione della riproduzione delle zanzare alla fonte (rimozione e modifica dei siti di riproduzione) e riducendo il contatto tra le zanzare e le persone.
• Ciò può essere ottenuto riducendo il numero di raccolte d'acqua naturali e artificiali che contengono le larve della zanzara, riducendo le popolazioni di zanzare adulte vicine alle comunità a rischio con barriere quali zanzariere, porte e finestre chiuse, abiti lunghi e repellenti.
Prevenzione dell’infezione da virus Zika
• Dal momento che le zanzare Aedes pungono di giorno, si raccomanda a chi dorme durante il giorno, soprattutto bambini, malati o anziani, di riposare sotto zanzariere trattate con o senza insetticidi.
• L’irrorazione aerea può essere effettuata utilizzando gli insetticidi adeguati (raccomandati dallo Schema di Valutazione sui Pesticidi, a cura dell’OMS) possono essere utilizzati anche come larvicidi per trattare raccoglitori di acqua relativamente grandi, quando tecnicamente indicato.