Conseguenze a lungo termine della prematurità e del basso peso per l’età gestazionale :...
-
Upload
scott-barrett -
Category
Documents
-
view
219 -
download
0
Transcript of Conseguenze a lungo termine della prematurità e del basso peso per l’età gestazionale :...

Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :• ComportamentaliComportamentali• EndocrineEndocrine• MetabolicheMetaboliche• RespiratorieRespiratorie
Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :• ComportamentaliComportamentali• EndocrineEndocrine• MetabolicheMetaboliche• RespiratorieRespiratorie
Angelo PietrobelliClinica Pediatrica, Università degli Studi di Verona
Nicola Fuiano Pediatria e Allergologia Pediatrica ASL della Provincia di Foggia

Early-life origins of adult disease: national longitudinal population-based study of the United States.
Johnson RC, Schoeni RF. Am J Public Health 2011 Dec;101(12):2317-24
Aim:
To examine the relation between low birth weight (LBW) and childhood family and neighborhood socioeconomic disadvantage and disease onset in adulthood.
Study population:
4378 children followed up to 2007 (when they were aged 39 up to 56 years).
Conclusions:
LBW plays an important role in disease onset.
O.R. by age 50 years
P <.01P <.01
P <.01 P
<.01

Change in prevalence of chronic conditions between childhood
and adolescence among extremely low-birth weight children.
Hack M et al. JAMA 2011 Jul 27: 306(4): 394-401
Aim:
To examine changes in the rates of chronic conditions between the ages of 8 and 14 years among extremely low-birth-weight (ELBW) children compared with normal-birth-weight (NBW) controls.
Study population:
Cohort study conducted from 2004 through 2009:
181 ELBW (weight < 1 kg) and 125 NBW controls of similar sociodemographic status born from 1992 through 1995 in Cliveland, Ohio.
Main outcome measures:
Rates of chronic conditions overall (measured with the revised Questionnaire for identifying Children With Chronic Conditions) and rates of asthma and obesity.
75
37
74
47
ELBW NBW
Chronic conditions
age 8 years age 14 years
%

Change in prevalence of chronic conditions between childhood
and adolescence among extremely low-birth weight children.
Hack M et al. JAMA 2011 Jul 27: 306(4): 394-401
Logistic regression
(adjusted for sociodemographic status,
sex, and race):
ELBW children continued to
have a higher rate of chronic
conditions than NBW controls
at age 14 years.

Asthma requiring medication
Change in prevalence of chronic conditions between childhood
and adolescence among extremely low-birth weight children.
Hack M et al. JAMA 2011 Jul 27: 306(4): 394-401
%
P = .002
%
Differences in rates of asthma at age of 14 years

Change in prevalence of chronic conditions between childhood
and adolescence among extremely low-birth weight children.
Hack M et al. JAMA 2011 Jul 27: 306(4): 394-401
0.38 –
0.06 –
0
Mean z scores for Body Mass Index
in ELBW children(P < .001)
at age 8 years
at age 14 years
%

Change in prevalence of chronic conditions between childhood
and adolescence among extremely low-birth weight children.
Hack M et al. JAMA 2011 Jul 27: 306(4): 394-401
Results: the scores and rates did not change among NBW
controls such that at the age of 14 years the differences between
ELBW and NBW children in mean z scores for body mass index
(0.38 vs 0.56, respectively; adjusted mean difference -0.2 [95% CI,
-0.5 to 0.1]) or rates of obesity (19% vs 20%, respectively; AOR,
1.1 [95% CI, 0.6 to 2.0]) were not significant.
Conclusions: among ELBW children, rates of
overall chronic conditions and asthma did not change between the
ages of 8 and 14 years but the rate of obesity increased.
Compared with NBW controls, the rates of chronic conditions were
higher but there were no significant differences in the rates of
asthma or obesity.

1.1. Preterm infantPreterm infant
2.2. Small for gestational Small for gestational
ageage
1.1. Preterm infantPreterm infant
2.2. Small for gestational Small for gestational
ageage

1. Preterm infant1. Preterm infant
Preterm Infant Preterm Infant : born <37 weeks’ gestationborn <37 weeks’ gestation
< 37 weeks: < 37 weeks:
““premature”premature”
“ “preterm”preterm”

DefinitionDefinition
Preterm infants are so different between each other.
Shorter is pregnancy more are risks’ factor for infants.
“Preterm”:
born between 34 and 36 weeks
of gestational age; “Moderate preterm”:
born between, 32 and 33 weeks
of gestational age; “Very low birth weight”:
born <32 weeks of gestational age; “Extremely very low birth weight”
born <28 weeks of gestational age.Linee guida della Società Italiana di Neonatologia

EpidemiologyEpidemiology
Preterm: Italy situation?Preterm: Italy situation?
40.000 preterm (6.9%) every year,
1 every 14 born, approximately 110/day;
VLBW: 5.500 year, 1 every 100 born.
first condition of death during first year of age.
Italy: 800 death/year
Dati della Società Italiana di Neonatologia

Premature babies – quality of lifePremature babies – quality of life
- Survival rate directly related to gestational age
- EVLBW (…- 24 - 26weeks) have survival rate close to 85%-10% VLBW health problems:
- brain,
- ROP,
- growth;
-Preterm infant: high level of SIDS and
high ER access.

2. Small for gestational age2. Small for gestational age
What is small for gestational age (SGA)?What is small for gestational age (SGA)?
Small for gestational age (SGA) is a term used to describe a baby who is smaller than the usual amount for the number of weeks of pregnancy. SGA babies usually have birth weights below the 10th percentile for babies of the same gestational age. This means that they are smaller than 90 percent of all other babies of the same gestational age. SGA babies may appear physically and neurologically mature but are smaller than other babies of the same gestational age; SGA babies may be proportionately small (equally small all over) or they may be of normal length and size but have lower weight and body mass; SGA babies could be premature (born before 37 weeks of pregnancy), full term (37 to 41 weeks), or post term (after 42 weeks of pregnancy).

Epigenetic regulation and fetal Epigenetic regulation and fetal programmingprogramming

Epigenetic regulation and fetal programming
Gicquel C. et al. Best Pract Clin Endocrinol Metab 2008 Fetal programming encompasses the role of developmental plasticity in response to environmental and nutritional signals during early life and its potential adverse consequences (risk of cardiovascular, metabolic and behavioural diseases) in later life. The first studies in this field highlighted an association between poor fetal growth and chronic adult diseases. However, environmental signals during early life may lead to adverse long-term effects independently of obvious effects on fetal growth. Adverse long-term effects reflect a mismatch between early (fetal and neonatal) environmental conditions and the conditions that the individual will confront later in life.
Fetal programming encompasses the role of developmental plasticity in response to environmental and nutritional signals during early life and its potential adverse consequences (risk of cardiovascular, metabolic and behavioural diseases) in later life. The first studies in this field highlighted an association between poor fetal growth and chronic adult diseases. However, environmental signals during early life may lead to adverse long-term effects independently of obvious effects on fetal growth. Adverse long-term effects reflect a mismatch between early (fetal and neonatal) environmental conditions and the conditions that the individual will confront later in life.

Epigenetic regulation and fetal programming
Adjusted for gestational age
Large for gestational age
Small for gestational age
• Premature (before 37 weeks of pregnancy)
• Full term (37 to 41 weeks of pregnancy)
• Post term (after 42 weeks of pregnancy))

Epigenetics and food allergyEpigenetics and food allergy
Hong X et al. Semin Immunopathol (2012) 34:655–669
Food allergy (FA), a major clinical and public health concern
worldwide, is caused by a complex interplay of • environmental exposures, • genetic variants, • gene environment interactions, • and epigenetic alterations.
Epigenetic alteration has been proposed as one of the
mechanisms to mediate the influence of early life
environmental exposures and gene–environment
interactions on the development of diseases later in life.

Epigenetics and food allergy
Prematurity is proposed to be associated with increased intestinal permeability and increased food antigen uptake which may lead to an increased risk of IgE mediated food allergy in premature children.
Robertson DM 1982 - Weaver LT 1984
Very low birth weight (LBW) preterm infants also are considered to have a wide range of immature digestive and absorptive functions, which might cause increased macromulecular absorption leading to food allergy.
McNeish AS 1984
Low birth weight (LBW) infants who received cow's milk formula developed latent systemic sensitization more rapidly than infants born at term.
Lucas A 1984

An Italian study compared 80 preterm infants with 80 sex-matched- and age-matched full-term infants at a mean age of 16 months and found no difference in frequency of positive skin tests to foods between the two groups.
De Martino M 1989
In the 1995 Manitoba birth cohort composed of 13,980 children: no association for prematurity and LBW with the risk of food allergy in childhood.
Liem IJ 2007
In the BBC: prematurity was associated with an increased risk of recurrent wheezing, but no such associations were found for either food allergy or eczema.
Kumar R 2008
Epigenetics and food allergy

A Japanese study: the prevalence of food allergy in LBW infants (8.1 %) was found to be significantly lower than in infants with normal birth weight at 18 months of age (11.2 %).
Hikino S 2001
Stressful intrauterine milieus (i.e., low birth weight) and genetic susceptibility to obesity synergistically affect adulthood risk of type 2 diabetes.
Case control study using 2591 type 2 diabetes and 3052 healthy control subjects.
Li Y et al 2012
Epigenetics and food allergy
2

Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :

Depression in young adults with very low birth weight: the Helsinki study of very low-birth-weight adults.
Räikkönen K et al. Arch Gen Psychiatry 2008; 65(3):290-6
Aim:
to test whether young adults aged 18 to 27 years with VLBW (<1500 g) differ from term control subjects in depression symptoms, current use of antidepressant medication and the rate of depression diagnosed by a physician.
Study population:
162 VLBW young adults (response rate 65.1%) and 172 term control subjects (response rate 54.8%) born between February 22.1978 and November 28.1985 in Helsinki.
Main outcome measures:
antidepressant use, history of physician-diagnosed, Beck Depression inventory score , and Center for Epidemiologic Studies Depression Scale Score.
- 29.1 - 20.1
95% CI
-53.7 to -8.4
95% CI
-40.8 to - 1.72
The VLBW participants reported 20.1% lower CES-D scores than the AGA
controls (P =.02), and 29.1% lower
than the controls (P =.004).
The VLBW participants reported 20.1% lower CES-D scores than the AGA
controls (P =.02), and 29.1% lower
than the controls (P =.004).

Depression in young adults with very low birth weight: the Helsinki study of very low-birth-weight adults.
Räikkönen K et al. Arch Gen Psychiatry 2008; 65(3):290-6
Results:
VLBW participants born appropriate for gestational age were 4.8 (95% CI, 1.3-10.0) times less likely to report a depression diagnosis than controls (P =.02).
In contrast, 52 VLBW participants born small for gestational age (birth weight < -2 SDs according to Finnish birth weight charts) reported 36.2% (95% CI, 1.1%-83.5%) higher Beck Depression Inventory scores (P =.04), were 4.0 (95% CI, 1.1-14.3) times more likely to use antidepressants (P =.03), and were 2.5 (95% CI, 1.0-6.3) times more likely to report a depression diagnosis (P =.04) compared with controls.
Conclusions: this is the first study (to our knowledge) to show that intrauterine growth pattern may modify associations between VLBW and depression. Intrauterine growth retardation rather than VLBW per se may pose a risk of depression in young adulthood.

Disabilities and health of extremely lowbirthweight teenagers:
a population-based study. Georgsdottir I et al. Acta Paediatr 2012; 101:518-23
Aim: evaluating of long-term outcome of
extremely low-birthweight (ELBW)
teenagers born in Iceland in 1991-95;Study population: 30 ELBW and 30 fullterm control;
age range 14-19 years;
assessed for
disabilities,
health problem,
learning difficulties.Results: a quarter of the ELBW teenagers had
disabilities.

Birth weight, stress, and symptoms of depression in adolescence: evidence of fetal programming in a
national canadian cohort.Colman I et al. Can J Psychiatry 2012 Jul;57(7):422-8.
Aim:
To investigate evidence of fetal programming in humans by studying whether adolescents born at high or low birth weights (LBW) are more likely to experience symptoms of depression and anxiety after experiencing stress.
Study population:
3732 members of a prospective Canadian cohort study assessed for symptoms of depression and anxiety at age 12 to 15 years (2006/2007),and had birthweight and gestational age (GA) data recorded in 1994/1995.
1.50
1.31The relation
between chronic stress and adolescent
depression and anxiety was more
pronounced in males who were
born SGA (interaction P <
0.05)
The relation between chronic
stress and adolescent
depression and anxiety was more
pronounced in males who were
born SGA (interaction P <
0.05)
95% CI
1.08 to 2.08
95% CI
0.99 to 1.72

School-age Outcomes of Extremely Preterm or Extremely Low Birth Weight Children.
Hutchinson EA et al. Pediatrics 2013; Apr;131(4):e1053-61.
Aim:
To monitor changes in the nature of neurobehavioral deficits in extremely preterm (EP) or extremely low birth weight (ELBW) survivors.
This study examines cognitive, academic, and behavioral outcomes at age 8 years for a regional cohort of EP/ELBW children born in 1997.
Setting:
The State of Victoria, Australia;Methods:
The EP/ELBW cohort comprised all live births with a gestational age <28 weeks (EP) or birth weight <1000 g (ELBW) born in 1997. Of 317 live births, 201 (63.4%) survived to 2 years of age. A term/normal birth weight (T/NBW) cohort was recruited comprising 199 infants with birth weights <2500 g or gestational age <37 weeks. Measures of intellectual ability, educational achievement, and behavior were administered at age 8.

Results:
The EP/ELBW group performed poorer than the T/NBW group on measures of IQ, educational achievement, and certain behavioral domains, even after adjustment for sociodemographic factors and exclusion of children with neurosensory impairment. The rate of any neurobehavioral impairment was elevated in the EP/ELBW group (71% vs 42%), and one-half of subjects had multiple impairments. The outcomes for those with <750 g birth weight or <26 weeks' gestational age were similar to those with a birth weight of 750 to 999 g or a gestational age of 26 to 27 weeks, respectively.
94.0
87.0
School-age Outcomes of Extremely Preterm or Extremely Low Birth Weight Children.
Hutchinson EA et al. Pediatrics 2013; Apr;131(4):e1053-61.
Retention percentage
Conclusions: despite ongoing
improvements in the management of EP/ELBW infants,
the rate of neurobehavioral
impairment at school-age remains too high relative to controls.
%

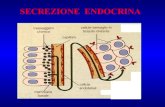
Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :

Serum thyroid hormone levels in healthy children from birth to adulthood and in short children born small for
gestational age. Lem A J et al. J Clin Endocrinol Metab 2012 Sep;97(9):3170-8.
Aim:
to obtain pediatric thyroid hormone reference ranges;
to investigate thyroid hormones in short SGA children before puberty, during puberty, and during postponement of puberty by GnRH analog;
and to evaluate thyroid hormones during GH treatment.
Patients and design:
in 512 healthy children (225 females; 0-18 yr), free T(4) (FT(4)), TSH, total T(4), T(3), rT(3), and T(4)-binding globulin were determined. Reference ranges were calculated using the linearity, median, and skewness method. In 125 short SGA children (62 females; mean age 11.3 yr), thyroid hormones were analyzed before and after 2 yr of GH treatment and additional GnRH analog.

Serum thyroid hormone levels in healthy children from birth to adulthood and in short children born small for
gestational age. Lem A J et al. J Clin Endocrinol Metab 2012 Sep;97(9):3170-8.
Results:
Thyroid references showed wide ranges postnatally and age-specific patterns thereafter, similar in boys and girls.
Untreated short SGA children had similar FT(4) and T(4) levels as the reference population but significantly higher T(3), rT(3), and T(4)-binding globulin levels.
During puberty and during GH treatment, FT(4) and rT(3) significantly decreased, whereas T(3) significantly increased.
Conclusion:
Age-specific thyroid reference ranges are presented. Puberty and GH treatment both induce changes in peripheral thyroid metabolism, resulting in more biologically active T(3) at the expense of less inactive rT(3), possibly mediated by IGF-I. GH treatment induces altered peripheral thyroid metabolism but does not result in thyroid dysfunction

Neonatal hyperthyrotropinemia is associated with low birth weight: a twin study.
Zung A et al. Eur J Endocrinol 2013 Jan 17;168(2):263-9
Background:
Contradictory reports ascribe neonatal hyperthyrotropinemia (HT) to prematurity or small weight for gestational age.
Aim:
To evaluate the association between neonatal HT and birth weight (BW), recovery rate of the disorder, and possible association with perinatal stress.
Study population:
2595 twin pairs that were screened both for TSH and thyroxine (T(4)) over 3 years were included.
Methods:
TSH and T(4) levels were evaluated along with BW, birth order, gender, and 17-hydroxyprogesterone (17OHP) that was considered as a surrogate marker for stress.

Neonatal hyperthyrotropinemia is associated with low birth weight: a twin study.
Zung A et al. Eur J Endocrinol 2013 Jan 17;168(2):263-9
Results:
Of all the twin pairs, 7.2% had neonatal HT.
Among 156 pairs, HT was more prevalent in the smaller twins (64%; P<0.001), especially in the discordant pairs (76%; P=0.001).
Seventy-five percent of the twins demonstrated a recovery within the first few weeks of life.
17OHP levels were similarly distributed between twins with and without HT.
In a cohort of 1534 twin pairs with normal thyroid function, mean TSH levels were significantly higher in the smaller than in the larger twin in the whole group (4.1±3.2 vs 3.8±2.9 mIU/l; P<0.001) and especially among discordant twins (4.7±3.4 vs 3.8±3.0 mIU/l; P<0.001).
Conclusions:
• Elevated TSH levels are associated with low BW both in infants with HT and in
normal neonates.
• A rapid recovery rate is expected in most cases.

Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :

Maternal and fetal cord blood lipids in intrauterine growth restriction.
Pecks U et al. J Perinat Med. 2012; 40 (3): 2387-96
Aim: small for gestational age neonates (SGA) could be subdivided into two groups according to the underlying causes leading to low birth weight.
Intrauterine growth restriction (IURG) is a pathologic condition with diminished growth velocity and fetal compromised well-being, while non-growth restricted SGA neonates are costitutionally (genetically determined) small.
Antenatal sonographic measurements are used to differentiate these two groups.
Maternal metabolic changes contribute to the pathogenesis of IUGR.
A disturbed lipid metabolism and cholesterol supply might affect the fetus, with consequences for fetal programming of cardiovascular diseases.
To evaluate fetal serum lipids and hypothesize a more atherogenic lipoprotein profile in IURG fetuses.

Maternal and fetal cord blood lipids in intrauterine growth restriction.
Pecks U et al. J Perinat Med. 2012; 40 (3): 2387-96
Methods:
umbilical cord serum lipids and oxidative modified, low-density
lipoprotein (oxLDL) concentrations were measured by colorimetric
enzymatic measurements, or by ELISA.
Three groups:
IUGR n. 36
SGA n. 22
CN (healthy, adequate for gestational age) n. 97

Maternal and fetal cord blood lipids in intrauterine growth restriction.
Pecks U et al. J Perinat Med. 2012; 40 (3): 2387-96
Results:Umbilical cord serum lipids
and oxidative modified,
low-density lipoprotein
(oxLDL) concentrations
measured by colorimetric
enzymatic measurements,
or by ELISA.
Three groups:
IUGR n. 36,
SGA n. 22,
CN (healthy, AGA) n. 97.
IUGR group
CN group
SGA group
Fetal•HDL-C
(P < 0.001)•TC
(P< 0.01)
Atherogenic indices
oxHDL/LDL-C ratio
(P < 0.001)
CN groupIUGR group
Conclusions:
A disturbed cholesterol supply in IURG fetuses;
Born SGA has been shown to be a risk factor for developing cardiovascular disease later in life;
Since HDL-C has anti-inflammatory properties, a reduced HDL-C during fetal development, and an increase in atherogenic indices, might provide a link to this observation in IUGR fetuses.
Conclusions:
A disturbed cholesterol supply in IURG fetuses;
Born SGA has been shown to be a risk factor for developing cardiovascular disease later in life;
Since HDL-C has anti-inflammatory properties, a reduced HDL-C during fetal development, and an increase in atherogenic indices, might provide a link to this observation in IUGR fetuses.

Low birth weight as cardiometabolic risk in Japanese high school girls.
Mori M et al. J Am Coll Nutr. 2012 Feb;31(1):39-44.
Objective: to examine the relationships between birth weight and metabolic syndrome (MS) risk factors in healthy Japanese high school girls.
Methods: in 2007 and 2008, 243 healthy Japanese high school girls aged 16.4±1.4 years were examined:
anthropometric measurements (including WC),
SBP and DPB,
tryglicerides (TG), high-density lipoprotein cholesterol (HDL), insulin,
blood glucose to calculate insulin resistance after fasting for 3 hours
after lunch.

Results:
MS was detected in only
1 girl who had obesity
and 2 more risk factors
(high BP and high TG)
prevalence
Low birth weight as cardiometabolic risk in Japanese high school girls.
Mori M et al. J Am Coll Nutr. 2012 Feb;31(1):39-44.
%

Results:
180 girls reported their birth weight
Birth weights were significantly inversely related with:
SBP
DBP
TG
Insulin level
Insulin resistance
Number of metabolic risk factors
P = 0.007
P = 0.033
P = 0.050
P = 0.022
Low birth weight as cardiometabolic risk in Japanese high school girls.
Mori M et al. J Am Coll Nutr. 2012 Feb;31(1):39-44.
P = 0.009
P = 0.047

Results:
Thirteen girls (7,2 %) whose birth weights were lower than 2500
gr. had significantly higher:
SBP
DBP
TG
Insulin level
Insulin resistance
P = 0.037
P = 0.032
P = 0.043
Low birth weight as cardiometabolic risk in Japanese high school girls.
Mori M et al. J Am Coll Nutr. 2012 Feb;31(1):39-44.
P = 0.011
P =0.037
than 31 girls (17.2 %) with birth weights equal to or more than 3400 gr.

Conclusion:
The association of low birth weight could be detected to be significant with such risks factors of MS as :
SBP,
DBP,
TG,
insulin level,
and insulin resistance even in healthy Japanese school girls,
indicating the importance of follow-up and food educational programme for children with low birth weight for the prevention of MS in the later life.
Low birth weight as cardiometabolic risk in Japanese high school girls.
Mori M et al. J Am Coll Nutr. 2012 Feb;31(1):39-44.

Objective: we hypothesized that, as compared with a matched control group at term, young adults with very low birth weight (VLBW < 1.5 kg) would have higher 24-hour ambulatory blood pressure.
Ambulatory blood pressure in young adults with very low birth weight.
Hovi P et al. J Pediatr 2010 Jan;156(1):54-59.
Study design: in the greater Helsinki area: two groups of subjects:
1. 118 18- to 27-year-old subjects born with VLBW,
the mean birth weight was 1.1 kg [± 0.2],
the gestational ages were 29.2 [± 2.3]
2. 120 term-born subjects, with similar age, sex, and birth hospital,
the mean birth weight was 3.6 kg [± 0.5],
the gestational ages were 40.1 [± 1.0].

Methods:Current education of higher-
educated parents served as an indicator of childhood socioeconomic status.
Ambulatory blood pressure was measured during a 24-hour period with an oscillometric device.
Ambulatory blood pressure in young adults with very low birth weight.
Hovi P et al. J Pediatr 2010 Jan;156(1):54-59.
Prevalence of hypertension in the two groups of subjects
Results:
VLBW subjects had, with sex, age, and body mass index adjustment,a 2.4 mmHg (95 % confidence interval, 0.2 to 4.6)
• when socioeconomic status was taken
into account, results remained unchanged
Conclusion:
Higher rates of hypertension and higher 24-hour blood pressure among young adults with VLBW may indicate higher risk for adverse cardiovascular outcomes
Conclusion:
Higher rates of hypertension and higher 24-hour blood pressure among young adults with VLBW may indicate higher risk for adverse cardiovascular outcomes

Objective: to evaluate the association between birth weight and
blood pressure (BP) in healthy 9- to 10-year-old Icelandic
children.
The relationship between birth weight and blood pressure in childhood: a population-based study.
Steinthorsdottir SD et al. Am J Hypertens. 2013 Jan;26(1):76-82.
Methods: each child underwent 4 seated BP measurements, and
the BP percentile was calculated from the mean of the 4
measurements. Height and weight were measured and birth
weight retrieved from the Icelandic Birth Registry.
Birth measures and anthropometric data were correlated with BP
and BP percentiles. Multivariable linear regression was employed
to examine the association between BP and birth measures.

Results: of 857 children with complete data, 445 were female (51.9%). The mean BP was 112/64 mm Hg in males and 111/63 mm Hg in females. The mean birth weight was 3714 ± 620 g.
No correlation was found between birth weight and absolute BP values. A significant negative correlation between birth weight and both systolic (r = -0.09, P = 0.005) and diastolic (r = -0.08, P = 0.014) BP percentiles was observed. Gestational age did not correlate with BP.
Conclusion: in contrast to many previous studies, we found no association between birth weight and absolute BP in children. However, we observed a statistically significant negative correlation between birth weight and BP percentiles. The lack of standardized BP values may partly explain the conflicting results of previous studies in children, and we suggest that BP percentiles be examined more thoroughly in association with birth weight.
The relationship between birth weight and blood pressure in childhood: a population-based study.
Steinthorsdottir SD et al. Am J Hypertens. 2013 Jan;26(1):76-82.

Effect of pregnancy for females born small on later life
metabolic disease risk. Tran M et al. PLoS One 2012;7(9):e45188. Erratum in: PLoS One.
2012;7(11)
Background:
there is a strong inverse relationship between a females own birth weight and her subsequent risk for gestational diabetes with increased risk of developing diabetes later in life. We have shown that growth restricted females develop loss of glucose tolerance during late pregnancy with normal pancreatic function.
Aim:
to determine whether growth restricted females develop long-term impairment of metabolic control after an adverse pregnancy adaptation. Uteroplacental insufficiency was induced by bilateral uterine vessel ligation (Restricted) or sham surgery (Control) in late pregnancy (E18) in F0 female rats.

Effect of pregnancy for females born small on later life
metabolic disease risk. Tran M et al. PLoS One 2012;7(9):e45188. Erratum in: PLoS One.
2012;7(11)
Methods:
Uteroplacental insufficiency was induced by bilateral uterine vessel ligation (Restricted) or sham surgery (Control) in late pregnancy (E18) in F0 female rats.
F1 Control and Restricted female offspring were mated with normal males and allowed to deliver (termed Ex-Pregnant).
Age-matched Control and Restricted Virgins were also studied and glucose tolerance and insulin secretion were determined.
Pancreatic morphology and hepatic glycogen and triacylglycerol content were quantified respectively.

Effect of pregnancy for females born small on later life
metabolic disease risk. Tran M et al. PLoS One 2012;7(9):e45188. Erratum in: PLoS One.
2012;7(11)
Results:
Restricted females were born lighter than Control and remained lighter at all time points studied (p<0.05). Glucose tolerance, first phase insulin secretion and liver glycogen and triacylglycerol content were not different across groups, with no changes in β-cell mass. Second phase insulin secretion was reduced in Restricted Virgins (-34%, p<0.05) compared to Control Virgins, suggestive of enhanced peripheral insulin sensitivity but this was lost after pregnancy. Growth restriction was associated with enhanced basal hepatic insulin sensitivity, which may provide compensatory benefits to prevent adverse metabolic outcomes often associated with being born small. A prior pregnancy was associated with reduced hepatic insulin sensitivity with effects more pronounced in controls than Restricted.
Conclusion:
Our data suggests that pregnancy ameliorates the enhanced peripheral insulin sensitivity in growth restricted females and has deleterious effects for hepatic insulin sensitivity, regardless of maternal birth weight.

Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :

Occurrence and severity of bronchopulmonary
dysplasia and respiratory distress syndrome after a preterm birth.
Landry JS et al. Paediatr Child Health2011 Aug;16(7):399-403.
Background: bronchopulmonary dysplasia (BPD) remains an important complication of preterm birth, frequently resulting in prolonged hospital stay and long-term morbidity.
Setting: Montreal Children's Hospital (Montreal, Quebec).
Subjects: a historical cohort study of all preterm infants (gestational age younger than 37 weeks) admitted between January 1, 1980, and December 31, 1992.
Methods: information collected included demographic data, maternal and perinatal history, and main neonatal outcomes. Independent risk factors associated with BPD were identified by univariate analysis using one-way ANOVA, t tests or Mantel-Haenszel χ(2) testing. Severity of disease was studied using an ordinal multinomial logistic regression model.

Occurrence and severity of bronchopulmonary
dysplasia and respiratory distress syndrome after a preterm birth.
Landry JS et al. Paediatr Child Health2011 Aug;16(7):399-403.
Results: 1192 preterm infants were admitted, of whom 551 developed respiratory distress syndrome , and 322 developed BPD. For each additional week of prematurity, the risk of developing BPD increased by 54% (adjusted OR 1.54/week [95% CI 1.45 to 1.64]). For each point subtracted on the 1 min Apgar score, the risk of developing BPD was increased by 16% (OR 1.16 [95% CI 1.1 to 1.3]).
BPD was also associated with the presence of patent ductus arteriosus (OR 3.5 [95% CI 2.1 to 6.0]), pneumothorax in the first 48 h (OR 9.4 [95% CI 3.6 to 24.8]) or neonatal pneumonia/sepsis in the neonatal period (OR 1.9 [95% CI 1.1 to 3.2]). Severity of BPD was associated with gestational age, 1 min Apgar score, very low birth weight and the presence of neonatal pneumonia/sepsis.
Conclusions:factors associated with BPD following a
preterm birth were
the degree of prematurity,
birth weight,
Apgar score at 1 min,
and the presence of patent ductus arteriosus,
pneumothorax
or neonatal pneumonia/sepsis

Short term outcomes after extreme preterm birth in England:comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). Costeloe KL et al. BMJ 2012 Dec 4;345:e7976
Objective: To determine survival and neonatal morbidity for babies born between 22 and 26 weeks’ gestation in England during 2006, and to evaluate changes in outcome since 1995 for babies born between 22 and 25 weeks’ gestation.
Setting: Maternity and neonatal units in England. Participants: 3133 births between 22 and 26 weeks’ gestation in 2006; 666 admissions to neonatal units in 1995, 1115 admissions to neonatal units in 2006, of babies born between 22 and 25 weeks’ gestation. Main outcome measures: Survival to discharge from hospital, pregnancy and delivery outcomes, infant morbidity unit discharge.

Results:
Survival
of live born
babies
in 2006
P < 0.001
Short term outcomes after extreme preterm birth in England:comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). Costeloe KL et al. BMJ 2012 Dec 4;345:e7976
%

Short term outcomes after extreme preterm birth in England:comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). Costeloe KL et al. BMJ 2012 Dec 4;345:e7976
Results:
in 2006
at discharge
from hospital:
%

Short term outcomes after extreme preterm birth in England:comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). Costeloe KL et al. BMJ 2012 Dec 4;345:e7976Results: for babies born between 22 and 25 weeks’ gestation
from March to December
+44.0 %
P < 0.001
%

Short term outcomes after extreme preterm birth in England:comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). Costeloe KL et al. BMJ 2012 Dec 4;345:e7976
Results: The proportions of babies surviving in 2006 with
bronchopulmonary dysplasia, major cerebral scan
abnormality, or weight and/or head circumference < - 2SD were
similar to those in 1995, but the proportion treated for
retinopathy of prematurity had increased from 13 % to 22 %
( P = 0.006 ).
Predictors of mortality and morbidity were similar in both
cohorts.
Conclusions:
Survival of babies born between 22 and 25 weeks’ gestation has increased since 1995 but the pattern of major neonatal
morbidity and the proportion of survivors affected are unchanged.
These observations reflect an important increase in the number of preterm
survivors at risk of later health problems.

Predictors for asthma at age 7 years for low-income children enrolled in the Childhood Asthma Prevention
Study. Tamesis GP et al. J Pediatr2013 Mar;162(3):536-542.e2.
Objective:
To identify the predictive factors of early childhood wheezing in children of low socioeconomic status.Study design:
The Childhood Asthma Prevention Study Participants:
177 low-income children (9-24 months old) with frequent wheezing.
At age 7 years, presence of asthma was assessed through caregiver reports of physician diagnosis of asthma (CRPDA) and corroborated by assessment of bronchial hyperresponsiveness (BHR).
Lung function, inflammatory markers, and asthma symptom severity were compared for children with ±CRPDA, ±BHR, and asthma.
Baseline predictors for CRPDA, BHR, and asthma at 7 years of age were examined.

Predictors for asthma at age 7 years for low-income children enrolled in the Childhood Asthma Prevention
Study. Tamesis GP et al. J Pediatr2013 Mar;162(3):536-542.e2.
Results:
Maternal symptom report strongly differentiated children with +CRPDA (49%) despite comparable airflow measurements (P < .0001), and spirometric lung function measurements were different for +BHR (65%) versus -BHR (P < .005). Univariate analyses revealed different baseline predictors of +CRPDA and +BHR for children at age 7 years. Higher levels of maternal psychological resources were associated with +CRPDA, but not +BHR.
Only 39% of children with a history of frequent wheezing met the conservative definition of asthma at age 7 years, with the following significant predictors found: low birth weight, baseline symptom severity, and maternal psychological resources.
Conclusions: this low-income, multi-ethnic group of wheezing infants
represents a unique population of children with distinct characteristics and risks for
persistent asthma.
Determination of asthma status at 7 years of age required objective measurement of
BHR in addition to CRPDA.
The association of maternal psychological resources with +CRPDA may represent a
previously unrecognized factor in the determination of asthma status among
low-income groups

Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :• ComportamentaliComportamentali• EndocrineEndocrine• MetabolicheMetaboliche• RespiratorieRespiratorie
Conseguenze a lungo termine della Conseguenze a lungo termine della prematurità prematurità
e del basso peso per l’età gestazionale :e del basso peso per l’età gestazionale :• ComportamentaliComportamentali• EndocrineEndocrine• MetabolicheMetaboliche• RespiratorieRespiratorie
? Take home ? Take home messagemessage

Pregnancy complications among women born preterm. Boivin A et al. CMAJ 2012 Nov 6;184(16):1777-84.
Aim:
to examined the relation between preterm birth and pregnancy
complications later in life.
Methods:
in the province of Quebec: 7405 women born preterm (554 < 32
weeks, 6851 at 32-36 weeks) and a matched cohort of 16 714
born at term between 1976 and 1995 who had a live birth or
stillbirth between 1987 and 2008. The primary outcome measures
were pregnancy complications (gestational diabetes, gestational
hypertension, and preeclampsia or eclampsia).

Pregnancy complications among women born preterm. Boivin A et al. CMAJ 2012 Nov 6;184(16):1777-84.
Results
Overall, 19.9% of women born at less than 32 weeks, 13.2% born at 32-36 weeks and 11.7% born at term had at least 1 pregnancy complication at least once during the study period (p < 0.001).
Women born small for gestational age (both term and preterm) had increased odds of having at least 1 pregnancy complication compared with women born at term and at appropriate weight for gestational age.
After adjustment for various factors, including birth weight for gestational age, the odds of pregnancy complications associated with preterm birth was elevated by 1.95-fold (95% confidence interval [CI] 1.54-2.47) among women born before 32 weeks' gestation and 1.14-fold (95% CI 1.03-1.25) among those born at 32-36 weeks' gestation relative to women born at term.
INTERPRETATION:
• Being born preterm,
in addition to, and independent of,
being small for gestational age,
was associated with a significantly
increased risk of later having
pregnancy complications

Low birth weight and health expenditures from birth to late adolescence.
Hummer M et al. Eur J Health Econ 2013 Apr 2.
Objective:
to analyze the impact of low birth weight (LBW) and very low birth weight (VLBW) on health care utilization in childhood and early adolescence.
Data/methods
using Austrian health insurance administrative panel data linked to the Austrian birth register, we estimate the effects of LBW and VLBW in comparison to normal birth weight (NBW) on the number of days spent in the hospital and on expenditures for medical assistance and medical drugs among children and young adults between birth and 21 years of age. To account for the time-invariant heterogeneity of mothers, we control for sibling fixed effects.

Low birth weight and health expenditures from birth to late adolescence.
Hummer M et al. Eur J Health Econ 2013 Apr 2.
Results:
in comparison to their NBW counterparts, LBW infants spend
more days hospitalized and more is spent on medical drugs
(particularly on anti-infectives) for them in their first year of life.
Although the absolute differences in health service utilization
between NBW and LBW groups diminish over time, LBW newborns
still spend more days hospitalized, and their medical drug and
medical assistance expenses are significantly higher in early
childhood. During compulsory schooling, we observe a shift
toward diseases of the nervous system and mental and
behavioral disorders among children born with LBW. Some of
these effects persist until early adulthood.
Conclusion:
• We argue for further counseling efforts for expectant mothers on the determinants and
risk factors of LBW.
• Moreover, pre-school screenings especially tailored to LBW infants with a particular focus on mental health and behavioral
disorders can be easily integrated in the existing postnatal mother-child care program
in Austria to mitigate the consequences of negative conditions during pregnancy.