Emoglobinuria Parossistica Notturna: principi di terapia e ... · Emoglobinuria Parossistica...
Transcript of Emoglobinuria Parossistica Notturna: principi di terapia e ... · Emoglobinuria Parossistica...

Emoglobinuria Parossistica Notturna: principi di terapia e ruolo della rete
regionale
LANZA FRANCESCO
UOC EMATOLOGIA Lab. Specialistico
di Citometria e Cellule Staminali
Az Ospedaliera CREMONA

EPN
Malattia clonale di natura acquisita delle cellule staminali emopoietiche che
provoca:
1. Anemia dovuta ad emolisi intravascolare cronica e acuta;
2. Diatesi tromboembolica; 3. Leuco-piastrinopenia 4. Distonia della muscolatura liscia

Glicosil-Fosfatidil-Inositolo (GPI)
il glicosil-fosfatidil-inositolo (GPI) svolge un ruolo importante nell’ancoraggio di proteine che non possono entrare nella membrana lipidica per la mancanza di un segmento idrofobo sufficientemente esteso.
EPN

4
In PNH, GPI-Deficient Cells Are Positively Selected in Pathologic Bone Marrow
Inoue N et al. Int J Hematol. 2003;77:107:107-112.
RBCs
Monocytes
Platelets
Granulocytes
Lymphocytes
Step 1 Step 2
Hematopoie9c Stem Cells
RBCs = red blood cells
GPI-‐Deficient Cell
Selected Cells*
GPI = glycerophosphatidylinositol.
Somatic Mutation in PIG-A
Immunologic Attack
Clonal Expansion by
Immuno-selection
Benign Tumor-Like Expansion
*Clones presumed to have a conferred growth advantage, in addition to the PIG-A mutation, resulting in GPI deficiency.

CLASSIFICATION OF HAEMOLYTIC ANAEMIAS
• Malaria • Auto-immune • Drug-induced • Micro-angiopathic • Other
Paroxysmal Nocturnal
Haemoglobinuria (PNH)
Acquired
Familial HUS (due to defective
C regulatory protein)
• emoglobinopathies • Enzimopathies • Membranopathies • Other
Hereditary
Extracorpuscolar causes
Intracorpuscolar causes

EPN: rilievi laboratoristici
• Anemia, reticolocitosi, <aptoglobina • Aumento del valore serico LDH (800-3000) • Citopenia: neutropenia, trombocitopenia • Emoglobinuria a poussee • “Perpetual Hemosiderinuria” • Segni di trombosi (dimero D) >40% pts • Aumento parametri di flogosi (infezioni) • Ipertensione polmonare • Insufficenza renale

EPN: Emoglobinuria

CD59, CD90, CD109
CD55 CD58 CD59 CD48 CD52 PrPc CD16
CD24 CD55
CD58 CD59 CD48 PrPC CD73 CD108
CD55 CD58 CD59 CD109 PrPC GP500 Gova/b
CD55 CD58 CD59 PrPC AChE JMH Ag Dombroch HG Ag
CD55 CD58 CD59 CD14 CD16 CD24 CD48 CD66b CD66c CD87 CD109 CD157 LAPNB1 PrPC p50-80 GPI-80 ADP-RT NA1/NA2
CD14 CD55 CD58 CD59 CD48 CD52 CD87 CD109 CD157 Group 8 PrPC GPI-80 CD16*
CD55 CD58 CD59 CD48 CD52 CD87 CD108 PrPc ADP-RT CD73 CD90 CD109 CD16
Haematopoietic Stem Cell
Platelets
RBC
Granulocytes
B cells
Monocytes
T cells
NK cells
Proteins deficient on PNH blood cells
Courtesy L. Del Vecchio

Granulocyte Lymphocyte
Monocyte Erythrocyte
CD66b
CD24
CD59 CD14
CD48
T
B
NK
Panel for cytometric analysis in patients with suspected PNH

Studio midollare in corso di EPN: procedura errata a fini diagnostici
FLAER Alexa-488

ERITROCITI
13.3%
FSC e SSC log

EPN: Monociti 3 popolazioni
CD33 CD45
CD14 CD14
I II III
CD64


The gold standard diagnos9c test for PNH is high sensi9vity flow cytometry performed on peripheral blood
• Tes%ng for PNH Iden%fies 3 Popula%ons of PNH Cells Type I: Cells with normal expression of CD59 Type II: PNH cells with par%al CD59 deficiency Type III: PNH cells with complete CD59 deficiency
• Granulocytes provide more accurate representa%on of PNH clone size
Percentages of PNH RBCs may be affected by hemolysis or blood transfusions
• Evaluate granulocytes and at least 1 addi%onal cell line: RBCs and/or monocytes
Borowitz MJ et al; Clinical Cytometry Society. Cytom B Clin Cytom. 2010;78:211-‐230
Standard Diagnostic Testing for PNH
14

15
Routine Testing Is Recommended for High-Risk Patient Populations
Two independent, interna9onal groups recommend tes9ng of high-‐risk pa9ents for PNH
Interna9onal Clinical Cytometry Society (ICCS) – provides laboratory tes%ng guidelines for rou%ne diagnosis of PNH
Interna9onal PNH Interest Group (I-‐PIG) – provides guidelines on diagnosis and management of PNH
1. Borowitz MJ et al; Clinical Cytometry Society. Cytometry B Clin Cytom. 2010;78:211-230.
2. Parker C et al; International PNH Interest Group. Blood. 2005;106:3699-3709.
Advancements in treatment op9ons warrant early diagnosis and interven9on Early diagnosis is essen9al for improved pa9ent prognosis1-‐2



REFERTAZIONE CASO I

Rule PNH In or Out Using High Sensitivity Flow Cytometry
and Clinical Assessment
Early Diagnosis Is Essen9al for Improved Pa9ent Management and Prognosis1-‐2
1. Borowitz MJ et al; Clinical Cytometry Society. Cytometry B Clin Cytom. 2010;78:211-230.
2. Parker C et al; International PNH Interest Group. Blood. 2005;106:3699-3709. 19
Unexplained Thrombosis
(venous or arterial)
Unexplained Cytopenia
RA-MDS (RCUD)
Aplastic Anemia Hemoglobinuria
Coombs-Negative Hemolytic
Anemia
RA-MDS= refractory anemia-myelodysplastic syndrome.

• PNH cells detected in 57% to 70% of AA1, 2, 3
• PNH cells detected in 20-‐50% of MDS pa9ents2,3
• PNH cells detected in 50% in other bone marrow
failure3
20
1. Sugimori C et al. BJH. 2009; 147: 102-12;
2. 2. Sugimori C et al. Blood. 2006 (107):1308-14; 3. 3. Galili N et al. JCO. 2009; Abstract 7082.
Co-‐evolu9on of PNH and BMF in a Hypoplas9c Marrow
Mutation of the PIG-A
AA / MDS

Suppor9ve Care Op9ons Do Not Impact Progression and Risk for Severe Morbidi9es and Mortality1
21
Historical care op9ons for PNH
• Transfusions1 – risk of iron overload • An%coagulants1 – ineffec%ve in many pa%ents
• Red cell supplements1 – may expand clone and elevate hemolysis
• Steroids/androgen hormones1 – adverse events
1. Parker C et al; Interna%onal PNH Interest Group. Blood. 2005;106:3699-‐3709.
THERAPY OF PNH

Bone Marrow Transplant (BMT) Is Associated With Significant Morbidi9es and Mortality2,3
22
Although it is the only poten9ally cura9ve therapy for PNH, BMT is associated with significant morbidi9es and mortality2,3
• In a study examining PNH pa%ents (n=23)2:
– 50% chronic grad-‐versus-‐host-‐disease (GVHD); 42% acute GVHD3
– 42% transplant-‐related mortality2 – \
• BMT has a significant impact on quality of life post-‐transplant4,5
1. Parker C et al; International PNH Interest Group. Blood. 2005;106:3699-3709. 2. Santaraone S et al. Haematologica. 2010;95:983-988. 3. de Latour PF et al. EBMT 2009:Abstract 316. 4. Bieri S et al. Bone Marrow Transplant. 2008;42:819-827. 5. Fraser CJ et al. Blood. 2006;108:2867-2873.

• Eculizumab binds with high affinity to C51,2
• Terminal complement - C5a and C5b-9 formation is blocked1,2
• Proximal functions of complement remain intact1,2 – Weak anaphylatoxin2,4
– Immune complex clearance2
– Microbial opsonization2
1. Soliris® (eculizumab) Summary of Product Characteris%cs. Cheshire, CT: Alexion Europe SAS. 2. Rother RP et al. Nature Biotechnol. 2007;25:1256-‐1264. 3. Walport MJ. N Engl J Med. 2001;344:1058-‐1066. 4. Figueroa JE, Densen P. Clin Microbiol Rev. 1991;4:359-‐395
Eculizumab is an An9-‐C5 An9body That Blocks Complement-‐Mediated Hemolysis
23

Eculizumab Clinical Development Program
Eculizumab (n = 11)
Eculizumab (n = 43)
Placebo (n = 44)
Eculizumab (n = 97)
Entered long-term extension (up to 3 years;
n = 10)
Entered long-term extension (up to 3 years;
n = 41)
Entered long-term extension (up to 3 years;
n = 44)
Entered long-term extension (up to 3 years;
n = 92)
Phase II pilot study NEJM 20041
(12 weeks) + 2 extension studies (52 and 104 weeks) 11 patients
Phase III study Blood 20083
SHEPHERD
(52 weeks) 97 patients
187 patients entered long-term extension trial4
Investigation: Measure clinical and biochemical indicators of hemolysis
Primary end points: stabilization of hemoglobin levels and the number of units of packed red blood cells
transfused
Primary efficacy end point: hemolysis as assessed by LDH
AEGIS study
Int J Hematol 20115
(12 weeks) 29 patients
Eculizumab (n = 29)
Primary end point: reduction of hemolysis
Entered long-term extension (up to 2
years; n = 27)
Phase III study NEJM 20062 TRIUMPH (26 weeks) 87 patients
Overview of the Eculizumab Clinical Development Program: Pilot Study, TRIUMPH, SHEPHERD, and AEGIS
1. Hillmen P et al. N Engl J Med. 2004;350:552-559. 2. Hillmen P et al. N Engl J Med. 2006;355:1233-1243. 3. Brodsky RA et al. Blood. 2008;111:1840-1847. 4. Hillmen P et al. Br J Haematol. 2013;162:62-73. 5. Kanakura Y et al. Int J Hematol. 2011;93:36-46.
24

25
1. Hillmen P et al. N Engl J Med. 2006;355:1233-‐1243. 2. Hillmen P et al. Blood. 2007;110:4123-‐4128. 3. Brodsky RA et al. Blood. 2008;111:1840-‐1847. 4. Hillmen P et al. Br J Haematol. 2013;162:62-‐73. 5. Socié G et al. 49th Annual Mee%ng of the American Society of Hematology; December 8-‐11, 2007; Atlanta, GA. Poster 891-‐III [Blood.007;110:3672.)
TRIUMPH1,2
• Patients not on Soliris (n = 44) • Soliris (n = 43) • Patients not on Soliris transitioned • to Soliris (n = 44)
SHEPHERD2
• Soliris (n = 97) EXTENSION studies • Hillmen 2013 (n = 189 and 87 at 72 and 144 weeks, respec%vely)4 • Socié 2007 (n = 10)5
Reduc9on in Hemolysis as Measured by LDH Was Sustained With Long-‐Term Soliris Treatment
Patients being treated with Soliris maintained an 86% reduction in hemolysis as measured by LDH over a 36-month treatment period4

Blood transfusion requirements in the 12 months before eculizumab therapy and the most recent 12 months on eculizumab treatment in 64 patients.
Kelly R J et al. Blood 2011;117:6786-6792 ©2011 by American Society of Hematology
Transfusion independence: 40 of 61 patients (66%)

Eculizumab Riduce l’Incidenza di Trombosi in Pazienti Trattati con Anticoagulanti1
! 94% di riduzione di incidenza di trombosi con SOLIRIS
(n=91)
P<0.001
*excludes patients on antiplatelet agents
1. Hillmen P, et al. Blood. 2007;110:4123-4128.

28
Soliris Treatment Resulted in Significant Improvements in Survival for Pa9ents With PNH
Years A[er Diagnosis
Pa9e
nts S
urviving (%
)
Actuarial Survival From the Time of Diagnosis in 80 Patients With PNH1
100
80
60
40
20
0 0 5 10 15 20 25
Age- and Gender- Matched Controls
Patients With PNH
Pa9ents With PNH on Soliris Compared With Age-‐ and Gender-‐Matched Controls2*
Time, (Years) Pa
9ents S
urviving, (%)
*Survival after 10-years is slightly inferior to controls with causes of
death related to bone marrow failure and not hemolysis or thrombosis
1. Hillmen P et al. N Engl J Med. 1995;333:1253-1258 2. Hill A et al. Presented at: 54th Annual Meeting of the American Society of Hematology (ASH); December 8-11, 2012; Atlanta, GA. Abstract 3472
Results from a 10-‐year mul9center observa9onal cohort study

29
• Treatment with Eculizumab resulted in a 92% reduc9on in thrombo9c events1
• Pa%ents being treated with Eculizumab reported significant improvement in evidence of pulmonary hypertension and dyspnea3,4
• 82% of pa%ents being treated with Eculizumab achieved transfusion independence at 36 months2
• Treatment with Eculizumab resulted in clinically meaningful improvements in quality of life, including reduced fa%gue and pain5
1. Hillmen P et al. Blood. 2007;110:4123-4128. 2. Hillmen P et al. Br J Haematol. 2013;162:62-73. 3. Hill A et al. Br J Haematol. 2012;158:409-414.
4. Hill A et al. Br J Haematol. 2010;149:414-425. 5. Hillmen P et al. N Engl J Med. 2006;355:1233-1243.
Clinical Efficacy of Eculizumab in Pa9ents With PNH

1. Hillmen P et al. N Engl J Med. 2006;355:1233-1243. 2. Brodsky RA et al. Blood. 2008;111:1840-1847. 3. Hillmen PD et al. Blood. 2007;110:4123-4128
4. Hill A et al. Br J Haematol. 2010;149:414-425. 5. Hillmen P et al. Am J Hematol. 2010;85:553-559. 6. Richards SJ et al. Blood. 2005;106:Abstract 1047.
7. Hillmen P et al. Br J Haematol. 2013;162:62-73. 8. Soliris® (eculizumab) summary of product characteristics. Cheshire, CT: Alexion Europe SAS. 9. Kelly RJ et al. Blood. 2011;117:6786-6792
Soliris Treatment Expecta9ons
30

REGIONE LOMBARDIA
PRESIDI REGIONALI DI RIFERIMENTO PER L’EPN:
CREMONA
MILANO
BERGAMO
BRESCIA
PAVIA
MONZA

Percorso Diagnos?co, Terapeu?co e Assistenziale (PDTA) rela?vo a: EMOGLOBINURIA PAROSSISTICA
NOTTURNA Codice esenzione RD0020

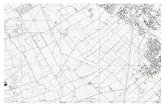
12,5 6,1 8,3 9,3
79,2 100,0 84,6
0
10
20
30
40
50
60
70
80
90
100
LOMBARDIA EMILIA-‐ROMAGNA ITALIA
%
Distribuzione della dimensione del clone
<1%
1-‐5%
>5%